Post Parturient Haemoglobinuria in Cattle: A Comprehensive Guide to PPH
Post-parturient haemoglobinuria (PPH), also known as Red Water Disease or Nutritional Hemoglobinuria, is a serious metabolic disorder affecting high-yielding dairy cattle and buffaloes. This guide covers its causes, symptoms, diagnosis, and treatment of post parturient haemoglobinuria in cattle.
What is Post Parturient Haemoglobinuria? Definition and Etiology
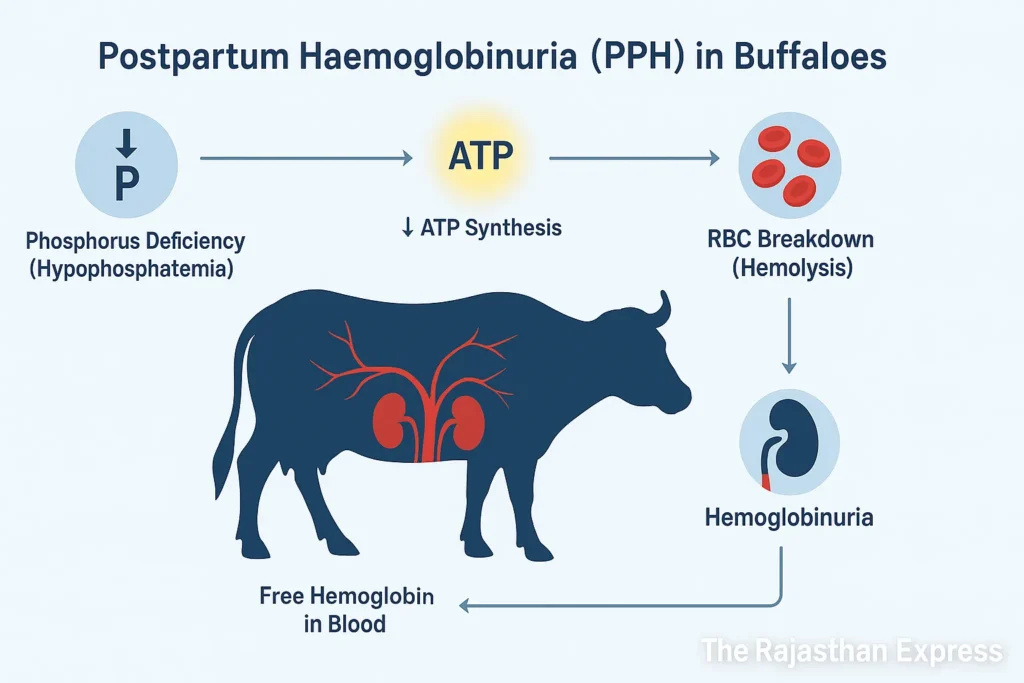
Post-parturient haemoglobinuria (PPH) is a sporadic disease primarily seen in high-yielding cows and buffaloes 2–4 weeks after calving. The disease occurs when lactation begins, and a phosphorus deficiency develops in the body.
This deficiency results in acute intravascular hemolysis, where red blood cells (RBCs) rupture, releasing their hemoglobin, which is then excreted through urine—a condition termed hemoglobinuria. This disease can cause severe anemia (blood deficiency). If not treated promptly, excessive blood loss can lead to the animal’s death.

Post-Parturient Haemoglobinuria (PPH)
| Also Known As | Red Water Disease, Nutritional Hemoglobinuria, Hypophosphatemia, Lahu Mutna |
|---|---|
| Definition | A sporadic metabolic disorder in high-yielding dairy cows and buffaloes, usually occurring 2–4 weeks after calving, characterized by acute intravascular hemolysis due to phosphorus deficiency, leading to hemoglobinuria, anemia, and risk of death if untreated. |
| Etiology & Pathophysiology | Severe phosphorus deficiency triggered by high milk output, soil-fodder mineral imbalances, excess dietary calcium/iron/aluminum, oxalates in feed, renal/liver disorders, or poor-quality fodders. Hypophosphatemia causes ATP depletion in RBCs, leading to hemolysis, anemia, and dark red urine. Also worsens hypocalcemia and milk fever through PTH–Vitamin D axis disruption. |
| Risk Factors |
|
| Clinical Presentations |
|
| Diagnosis |
|
| Differential Diagnoses |
|
| Treatment & Nursing Care |
|
| Prevention & Management |
|
| Prognosis | Good if treated promptly with phosphorus and supportive therapy. Severe cases with PCV < 15% or prolonged recumbency have guarded prognosis. Delay in treatment can lead to death from hemolytic anemia or renal damage. |
| Regulatory & Welfare Considerations | Animal welfare guidelines emphasize prevention of metabolic disorders through balanced feeding. In many countries (e.g., India, U.S.), veterinary extension programs recommend routine mineral supplementation to improve herd health and productivity. Non-ambulatory animals require special handling under OIE and national welfare standards. |
| Sources: Merck Veterinary Manual; ICAR-NDRI (India); FAO & OIE Livestock Health Guidelines; University Extension Services (Cornell, Iowa State) ; The Rajasthan Express | |
Main Causes of Phosphorus Deficiency in Cattle
The root cause is a severe dietary phosphorus deficiency, exacerbated by several factors.
1. During Milk Production:
The ratio of Calcium (Ca) and Phosphorus (P) in milk is approximately 1.3:1. A high production cow can lose more than 30-40 grams of phosphorus daily through milk. If the quantity of bioavailable (available) phosphorus in the diet is not sufficient or mineral mixture is not being given, then the cow goes into a state of negative phosphorus balance, due to which phosphorus deficiency occurs in her body.
2. Deficiency in Soil:
The deficiency of phosphorus in the soil has a direct impact on the phosphorus content of the fodder. In the absence of phosphorus-containing fertilizers (like DAP, SSP), deficiency of P occurs in the soil, due to which the quantity of phosphorus in the growing fodder will also be less. This is a major cause in countries like India. In the same way, the cause of a disease like Grass Tetany is also related to the soil.
3. The Soil-Plant-Animal Relationship:
The root cause of Grass Tetany (Hypomagnesemia) disease
Hypomagnesemic tetany is not only an animal disease; it is a soil-plant-animal metabolic related disorder. Its root cause is often hidden in the soil itself.
- Soil Factors: Acidic soil, high potassium (K) level and excessive use of nitrogen fertilizers reduce the availability of magnesium from the soil.
- Plant Factors: The fodder growing in such soil (like ryegrass, wheat) has very low quantity of magnesium (< 0.2%) and very high quantity of potassium (> 3.0%).
- Animal Factors: When animals eat this unbalanced fodder, then the absorption of magnesium in their stomach becomes even less, due to which its deficiency occurs in the blood and symptoms of tetany appear.
Read More About : Grass Tetany In Cattle
4. Mineral Imbalance:
Excessive quantity of calcium (Ca) in the diet disturbs the ideal ratio of Ca:P (approximately 2:1). This reduces the absorption of P. In the same way, iron (Fe) and aluminum (Al) form insoluble compounds with phosphate, due to which P becomes useless for the body.
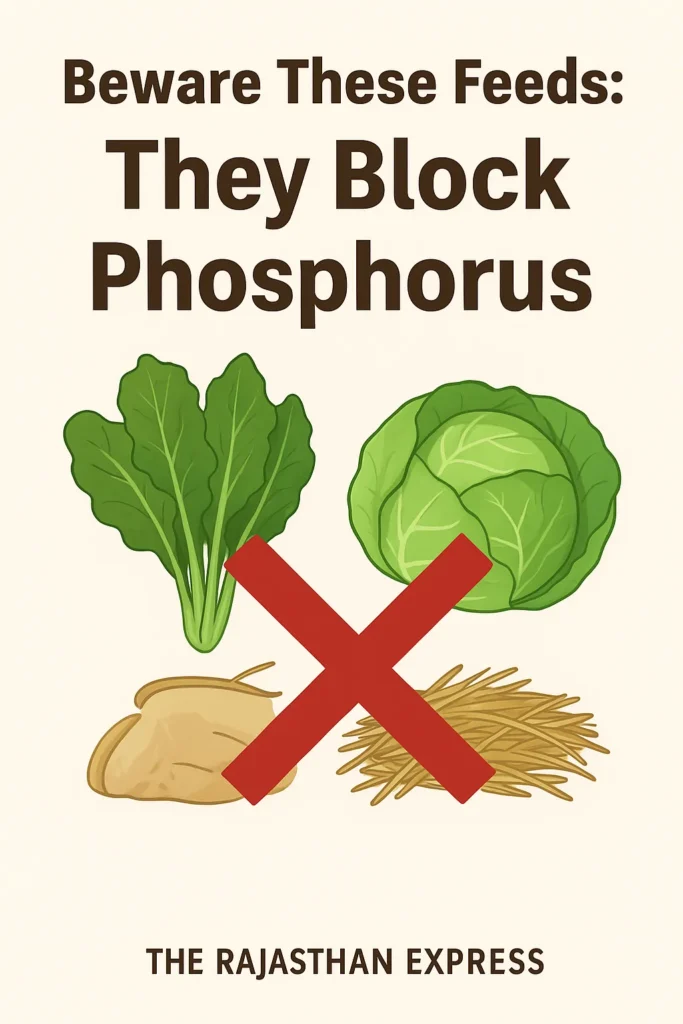
5. Absorption Interference:
Oxalates (found in cabbage, turnip) form bond with both phosphorus and calcium making them insoluble and inactive, due to which they are not absorbed from the intestines.
6. Metabolic Disorders:
Kidneys do reabsorption of phosphorus while filtering waste materials from the blood. When the functioning of kidney deteriorates, this process gets interrupted and P comes out in excessive quantity with urine. In the same way, diseases of liver affect the metabolism of Vitamin D, which is extremely necessary for the absorption of calcium and phosphorus.
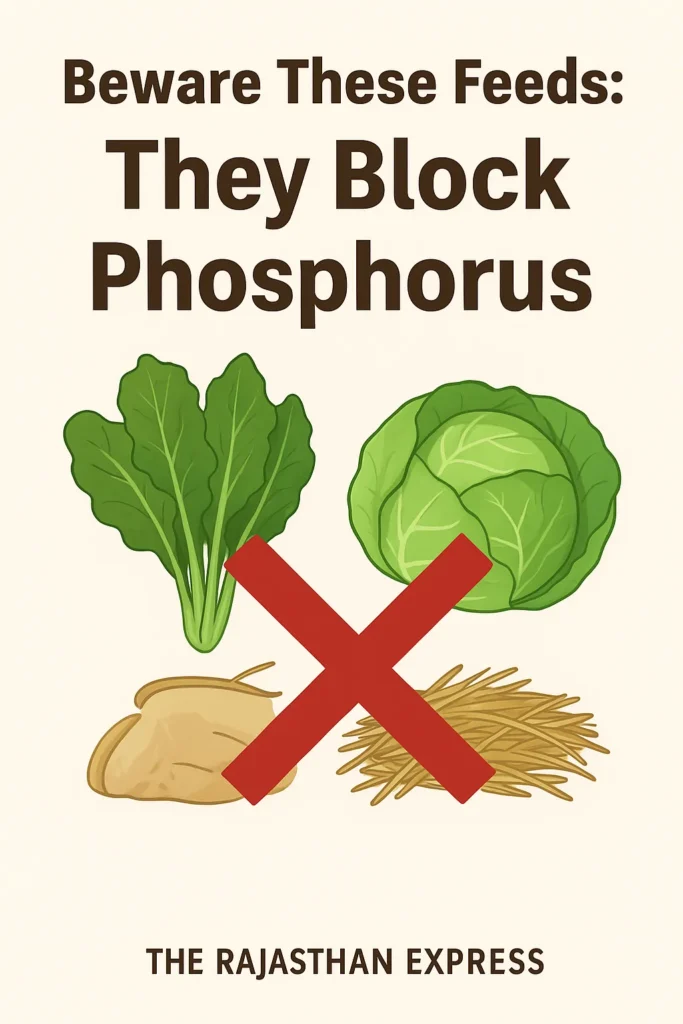
7. Certain Specific Fodders:
Some fodders can become the cause of phosphorus deficiency:
- Cabbage, Turnip: These contain high oxalates which bind phosphorus.
- Carrot and Brinjal leaves: The balance of nutrients in them is not right.
- Senji (Senji/Indian clover), Mustard leaves: These can have goitrogenic effect and Ca:P imbalance.
- Paddy straw, old hay/dry grass: The quantity of nutrition in them is less.
The quantity of phosphorus is less in these crops and they also hinder its absorption in the body.
🔎 Example: The Ca:P ratio is very high in Senji (Indian clover), due to which the absorption of phosphorus gets affected.
Metabolic Disease in Animals: Definition, Types, and Key Characteristics
Definition:
Metabolic Diseases are those diseases which occur due to deficiency, imbalance of nutrients, or disturbance of metabolism in the body. These diseases are especially related to milk production, pregnancy, and the energy requirements of the body.
Read More About : Metabolic Disease
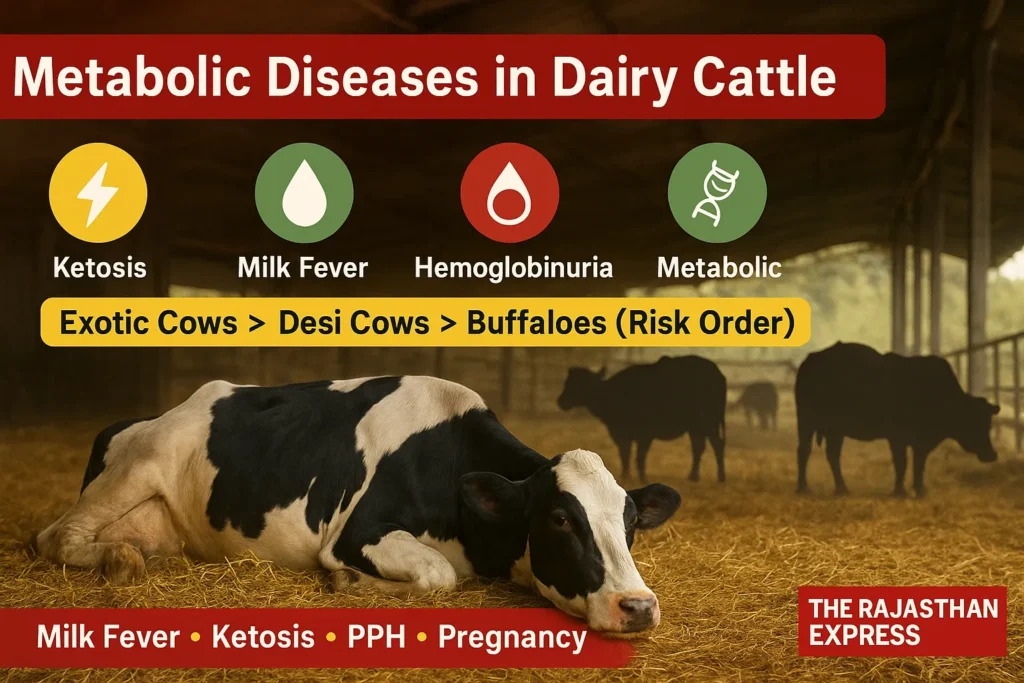
Main Features of Metabolic Disease in Dairy Cattle
- These diseases are Non-Contagious — do not spread from one animal to another.
- In most cases, these diseases are related to the production system, hence they are also called Production Diseases.
- Especially pregnant and milk-producing animals (like cow and buffalo) are more susceptible to these diseases.
- The possibility of metabolic diseases increases with increasing milk production.
- In native cows (Zebu cattle), the highest possibility of metabolic disease is found in the third calving.
- In exotic cows (Exotic Cattle), this possibility is highest in the fifth calving.
- In buffaloes, the possibility of metabolic diseases is mostly in the fourth calving.
- The order of possibility of metabolic diseases is as follows:
Exotic Cow > Native Cow > Buffalo - The possibility of Downer Cow Syndrome, Ketosis, Postpartum Haemoglobinuria, and Mastitis disease is higher in exotic cows, especially in the Holstein-Friesian breed.
- These same diseases are found mostly in the Sahiwal breed in native cows.
- The possibility of Milk Fever is highest in Jersey cows.
We have also explained these diseases in detail.
Explore the key metabolic diseases in cattle with quick links to each section:
- Milk Fever – Calcium deficiency immediately after calving
- Downer Cow Syndrome – Complications from prolonged lying after milk fever
- Ketosis In Cattle – Energy deficiency and ketone accumulation
- Postparturient Haemoglobinuria – Red blood cell destruction due to phosphorus deficiency
- Grass Tetany – Muscle cramps from magnesium deficiency
- Pregnancy Toxemia – Energy deficiency in late pregnancy
Advanced Research: The Relationship Between Phosphorus Deficiency and Milking Fever (PPH and Milk Fever)
Hypocalcemia, which is commonly called Milking Fever or Milk Fever, is a condition of massive drop in the level of calcium in the blood at the time of calving and after it. Although it is mainly associated with calcium deficiency, but now it has been found that not only calcium, but phosphorus deficiency (hypophosphatemia) also plays an important role in deepening this disease.
Read More About : Milk Fever In Cattle
Role of Hypophosphatemia:
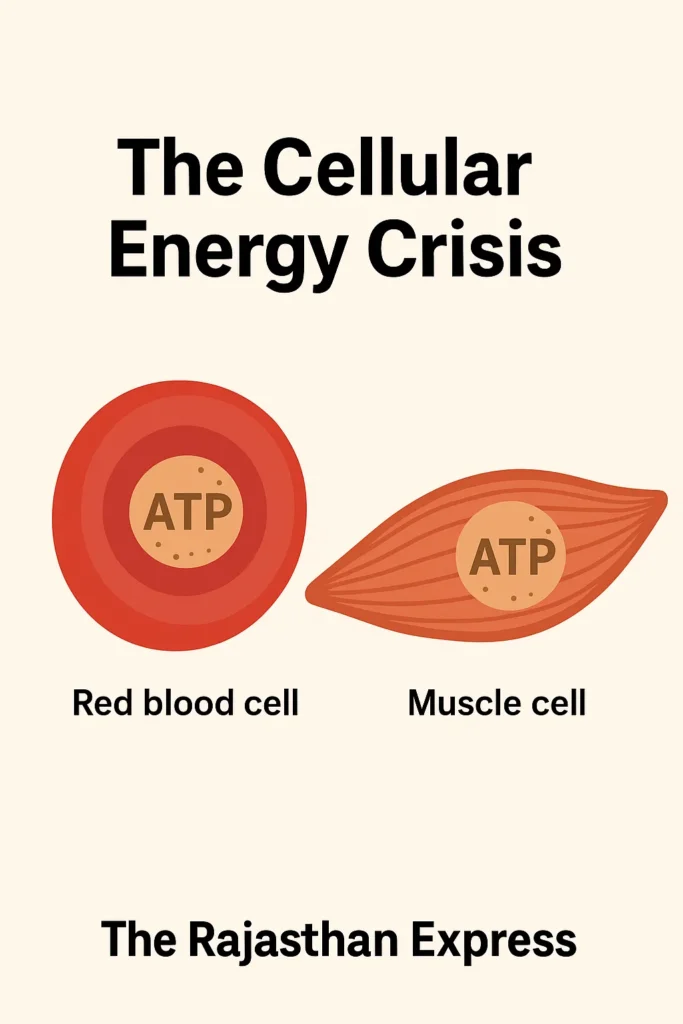
Hypophosphatemia (low phosphorus in blood) is also seen in approximately 80-90% of cows suffering from milk fever. Phosphorus is a very necessary element for the body because it helps in making ATP (Adenosine Triphosphate). ATP is the source of energy for the cells, like the moving battery of the body. When there is deficiency of phosphorus in the blood, then the ability to make energy (ATP) in the cells of the whole body decreases. This has two main serious consequences:
Main mechanism: Energy Crisis and Cellular Failure
Phosphorus is an essential component for the synthesis of Adenosine Triphosphate (ATP), called the “energy currency” of the cells. The low level of inorganic phosphate (Pi) in the blood seriously affects ATP production throughout the body. The most destructive impact is on two systems:
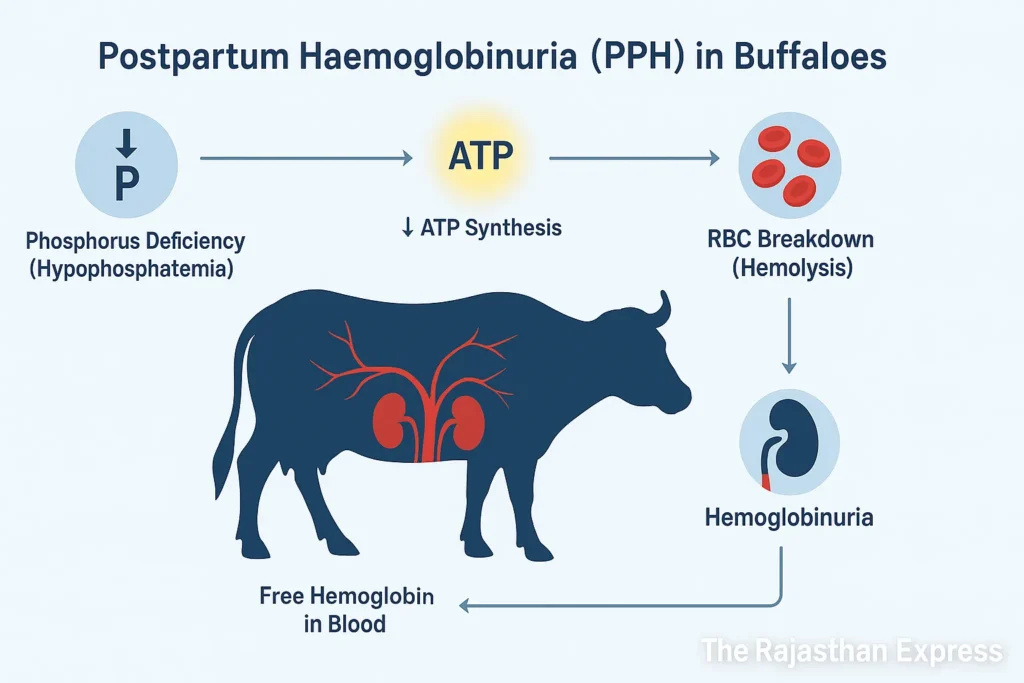
(a) Impact on Red Blood Cells (RBCs) and Hemolysis:
- Absence of Mitochondria: Mature RBCs do not have mitochondria, therefore they cannot produce ATP by oxidative phosphorylation. Their entire energy comes from Anaerobic Glycolysis (Embden-Meyerhof pathway).
- Glycolysis and the Role of Pi: The process of glycolysis is directly dependent on inorganic phosphate (Pi). On the deficiency of inorganic phosphate (Pi) glycolysis stops.
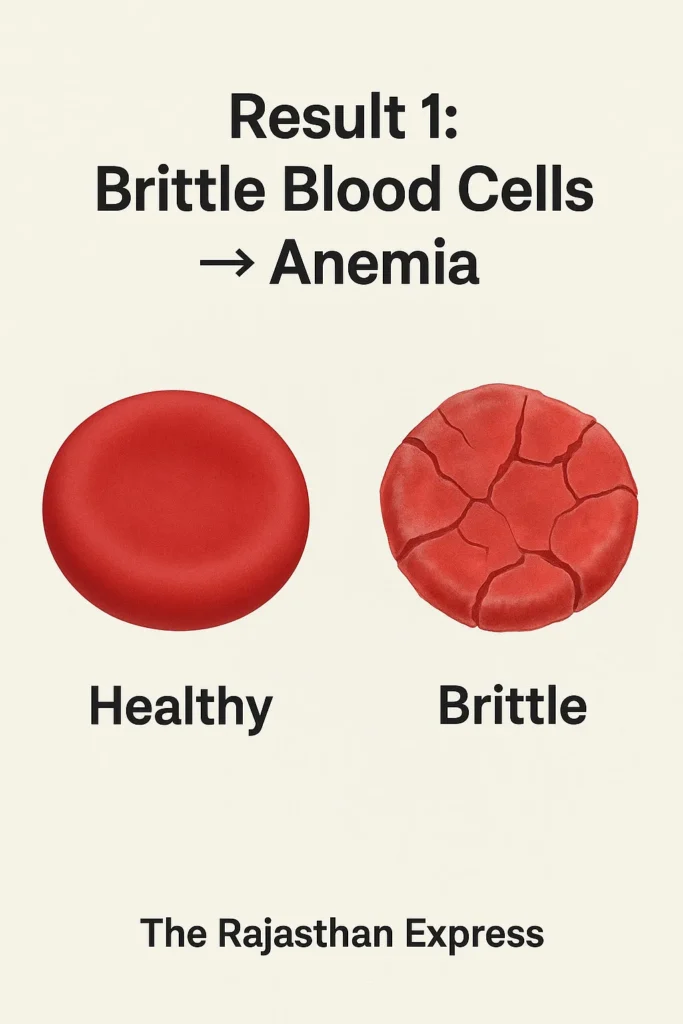
- ATP Deficiency: Deficiency of Pi reduces ATP production in RBCs dramatically.
- Hemolysis: The way of producing energy of the red blood cells (RBCs) has its own method, which depends entirely on phosphorus. When there is deficiency of phosphorus, the production of energy in these cells starts stopping. ATP is necessary to maintain the flexibility and integrity of the RBC membrane. It stabilizes the cell’s cytoskeleton by linking with proteins like spectrin and actin. Without this energy, these cells become weak and brittle and these break (lysis) easily while passing through narrow capillaries and spleen, due to which hemolysis happens. This causes anemia.
- Hemoglobinuria: Due to hemolysis, anemia (deficiency of blood) happens and the hemoglobin coming out from the broken cells comes out through urine, due to which the color of urine becomes dark like tea or coffee. This is a very serious symptom of PPH.
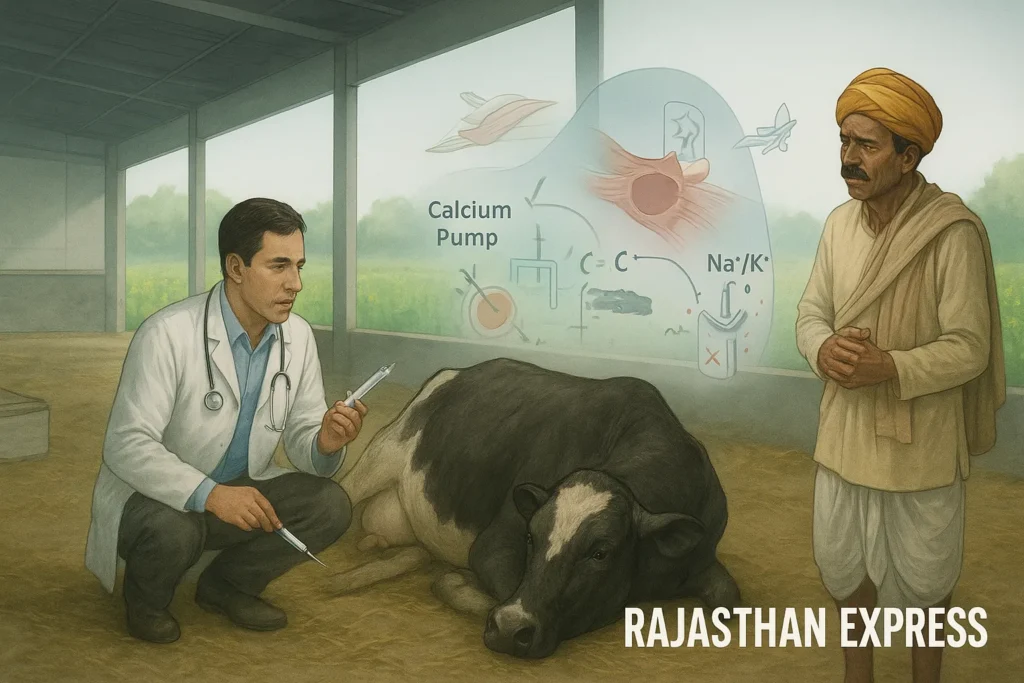
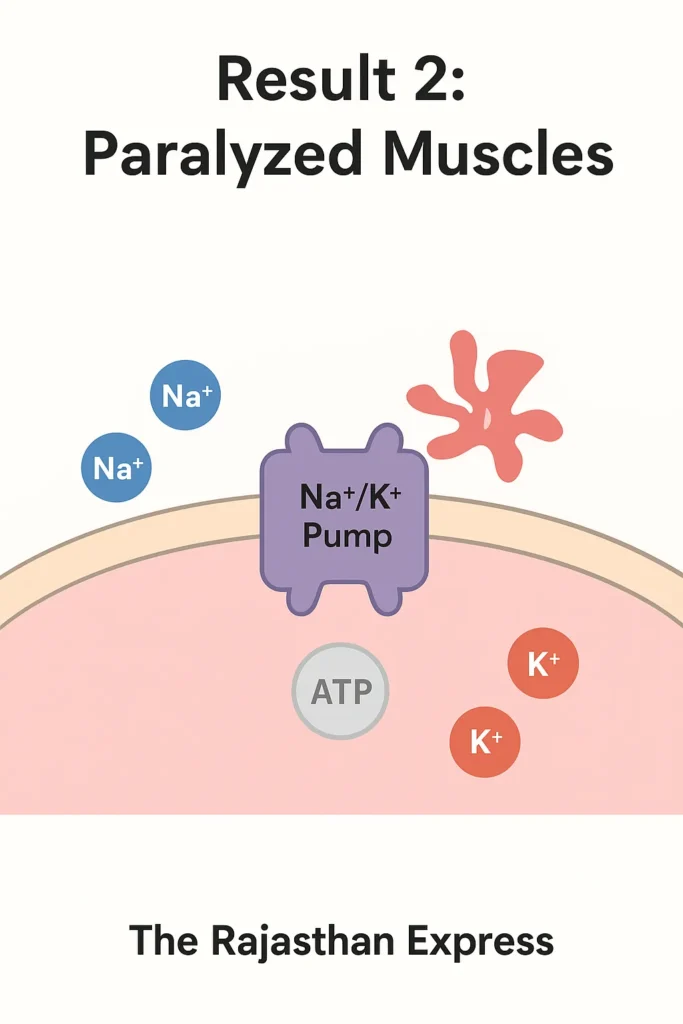
(b) Muscle Weakness and Paresis:
The most clear symptom of milk fever is muscle weakness and paralysis (paresis). This happens not only due to calcium deficiency, but also due to the energy crisis generated by phosphorus deficiency.
- ATP Requirement: Both the processes of contraction and relaxation of muscles require huge amount of ATP. Even the process of breathing is dependent on ATP.
- Consequences of ATP Deficiency:
- Dysfunction of Sarcoplasmic Reticulum: Deficiency of ATP prevents this organ from pumping calcium, due to which muscles do not work properly.
- Na⁺/K⁺ Pump Failure: The Na⁺/K⁺-ATPase enzyme of the cell membrane is dependent on ATP. On its failure, the functioning of muscles gets hindered, due to which flaccid paresis (loose paralysis) happens.
- In serious cases the cow is not able to stand (recumbency).
Key Points
PPH does not limit itself only to phosphorus deficiency and does not limit milk fever only to calcium deficiency, but transforms it into a complex metabolic crisis. It destroys red blood cells (RBCs) producing anemia and hemoglobinuria and hinders the functionality of muscles making weakness and the state of lying down (recumbency) even more serious. For this same reason, advanced treatment protocols of PPH often include combined injections of calcium and phosphorus, especially in those cases where the cow is not able to stand despite treatment.
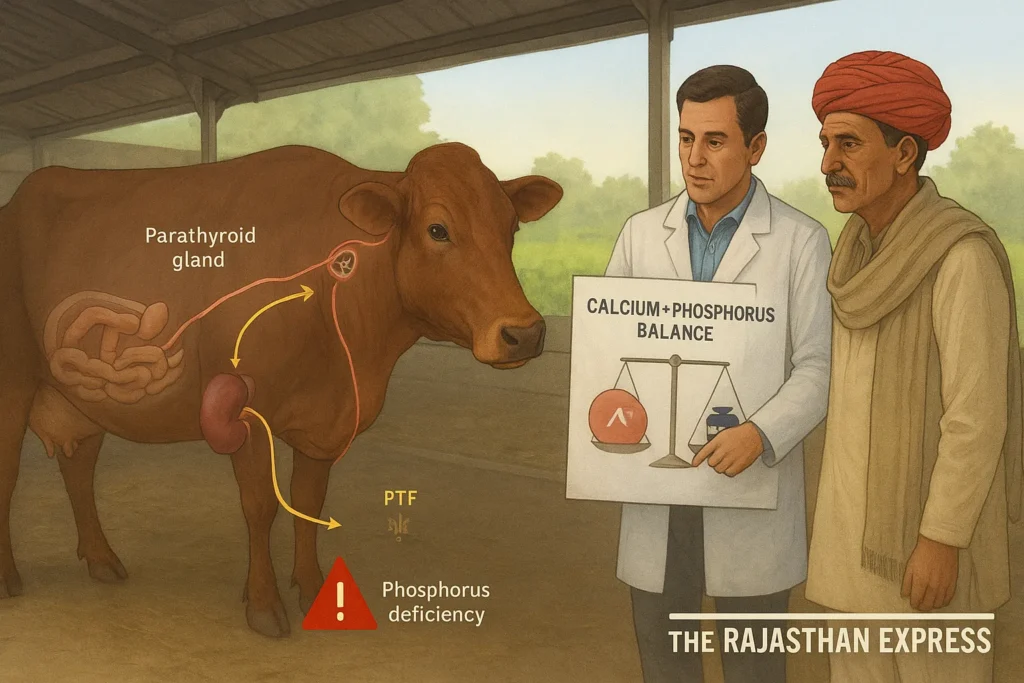
2. Hindrance in Parathyroid Hormone (PTH) Axis
When calcium is less in the blood, then the body releases parathyroid hormone (PTH). Its work is to increase the production of calcitriol (1,25-dihydroxy Vitamin D) in the kidney, which gets the absorption of calcium and phosphorus done from the intestines. But this hormone is able to work properly only when sufficient phosphorus is present in the body. If phosphorus itself is not there, then the body will not be able to give the necessary signals properly to fulfill the calcium deficiency. If there is deficiency of phosphorus in the diet, then PTH is not able to work effectively, because the formation of calcitriol gets affected. Due to this, the absorption of calcium decreases and the danger of milk fever increases even more.
3. Advanced Diagnostic and Management Strategies
Not only calcium in treatment: Only calcium borogluconate injection is given in traditional treatment. Modern research tells that combined injection of calcium and phosphorus can be more effective, especially in those cases where the cow does not get up even after treatment (“downer cow” cases).
- DCAD (Dietary Cation-Anion Difference) diet: Giving negative DCAD diet to cows 3-4 weeks before calving is the most effective strategy to prevent milk fever. It takes the body into a metabolic state which increases the sensitivity of tissues towards PTH and optimizes the metabolism of calcium and phosphorus.
- Blood gas analysis: In advanced veterinary centers, monitoring of Ca, P, Mg and pH in blood is done during treatment so that the treatment can be adjusted precisely.
Read More About : Downer Cow Syndrome In Cattle
Conclusion:
In today’s modern dairy farming, it is necessary to understand that milking fever is not just calcium deficiency. Phosphorus deficiency also plays an important role in generating and increasing this problem. Therefore, paying attention to both calcium and phosphorus for balanced diet for prevention of the disease and for treatment is extremely necessary for better health of the animal and productivity of the farm.
Alternative Names of Post-parturient Haemoglobinuria – PPH (Synonyms):
- PPH (Post-parturient Haemoglobinuria): This is the most common technical name.
- Lahu Mutna: Name prevalent in local language (लहू मूतना).
- Hypophosphatemia: Indicates the condition of phosphorus deficiency in blood, which is the root cause of this disease.
- Nutritional Haemoglobinuria: Emphasizes on dietary reasons.
- Red Water Disease: This name is used because the color of urine becomes dark red or like coffee, which happens due to the presence of hemoglobin in urine.
Predisposing Factors:
- Animals with high milk production capacity: This disease is especially seen in high milk production cows and buffaloes, because they lose very high quantity of phosphorus through milk.
- Unbalanced diet: Its biggest cause is the diet given to those animals which has less quantity of phosphorus or which hinder the absorption of phosphorus. Such diet includes the following:
- Turnip, carrot, brinjal leaves (high oxalate content)
- Senji (Indian Clover), mustard leaves (goitrogenic effect and Ca:P imbalance)
- Paddy straw, old dry hay or grass (low nutritional value and high fiber)
Clinical Signs of Post-parturient Haemoglobinuria
- Deficiency of phosphorus in the blood.
- Hemoglobinuria: The color of urine becoming dark red, brown or like coffee. This symptom happens due to the breaking of red blood cells within the blood vessels (Intravascular Hemolysis) and excretion of hemoglobin with urine.
- Decrease in appetite, weakness, and anemia (deficiency of blood).
- Fall in milk production.
- Yellowing of mucous membranes – this happens due to hemolysis and excessive loss of hemoglobin; jaundice can also be seen in serious cases.
- Increased heart and jugular vein beat.
- Dehydration – due to which hard, dry, brown dung, and problem of constipation happens.
- Heart and respiratory symptoms: Shortness of breath (Dyspnea) and increased heart beat (Tachycardia).
- Since PPH is a metabolic disease, therefore like other metabolic diseases, the body temperature remains normal or less in it also.
Advanced Research and In-Depth Analysis
1. The Theory of Cellular Energy Crisis:
According to traditional knowledge PPH is just phosphorus deficiency, but advanced research sheds light on the cellular energy crisis behind it.
- Importance of ATP: Phosphorus is absolutely essential for the construction of Adenosine Triphosphate (ATP). ATP is the “energy currency” of the cell, from which energy is received for every metabolic process of the body.
- Impact on Red Blood Cells (RBCs): The only source of energy production in mature RBCs is anaerobic glycolysis. This process is directly dependent on inorganic phosphate (Pi). On the deficiency of inorganic phosphate (Pi) in the blood, glycolysis stops, due to which the production of ATP in RBCs stops.
- Cause of Hemolysis: ATP is necessary to maintain the flexibility and integrity of the RBC membrane. Without ATP, RBCs become brittle and break easily in the blood flow, due to which hemolysis happens.
Read More About : DKA In Cats
2. Muscle Dysfunction:
The impact of phosphorus deficiency is not limited only to RBCs.
- ATP is also required for contraction and relaxation of muscles.
- Deficiency of ATP causes Na⁺/K⁺ Pump (Sodium-Potassium Pump) Failure, due to which the functioning of muscles gets hindered.
- Due to this, symptoms like extreme weakness, inability to stand (Recumbency), and flaccid paralysis appear in the animal, which are often understood only as symptoms of calcium deficiency.
3. Advanced Diagnostic and Therapeutic Approach:
- Blood Test (Blood Biochemistry): Instead of diagnosing only on the basis of symptoms, the levels of Inorganic Phosphorus (Pi), Calcium, Magnesium, and Hemoglobin in blood should be checked. Decreased PCV (Packed Cell Volume) confirms anemia.
- Combined Therapy: Only calcium injection is given traditionally. But, combined injection of calcium and phosphorus (like calcium phosphorus borogluconate) is advised in modern treatment protocols, especially in those cases where the animal does not get up even after treatment (“Downer Cow” Syndrome).
- Supportive Care: Blood transfusion and intravenous fluids (to correct dehydration) can be life-saving for animals suffering from serious anemia.
Normal Blood Parameters and Risk Levels
Normally, the blood P level in the body is 4 – 8 mg/dl. Falling below this indicates a phosphorus deficiency. The normal calcium-to-phosphorus ratio in a cow’s body is 2:1.
The normal levels of minerals in the blood of various animals are given in the following table:
| Normal Blood Parameters and Risk Levels in Different Species | ||||||
| Parameter | Units | Cattle | Buffalo | Sheep | Goat | Horse |
|---|---|---|---|---|---|---|
| Calcium | mg/dL | 8–12 | 8–14 | 11–13 | 9–12 | 10–13 |
| Phosphorus | mg/dL | 4–8 | 6–10 | 5–7 | 4–10 | 1–5 |
| Magnesium | mg/dL | 1–3 | 2–4 | 2–3 | 3–4 | 1–2 |
| Maintaining mineral balance is critical for preventing metabolic disorders in livestock. | ||||||
Diagnosis of PPH in Cattle
Diagnosis is based on a combination of clinical signs and laboratory tests.
- Key Clinical Signs: Dark coffee-colored urine in an animal in early lactation with signs of anemia.
- Phosphorus Levels:
- Affected animals: 0.4 – 1.5 mg/dL
- Normal animals: 4 – 8 mg/dL
| Critical Mineral Limits and Ratios in Ruminant Blood | |||
| Parameter | Normal Value | Tetany Risk Value | Critical Value |
|---|---|---|---|
| Serum Magnesium (Mg) | 1.8–2.5 mg/dL | 1.2–1.8 mg/dL | <1.2 mg/dL |
| Serum Calcium (Ca) | 8–10 mg/dL | 7–8 mg/dL | <7.0 mg/dL |
| Serum Inorganic Phosphorus (P) | 4.5–8.5 mg/dL | — | — |
| Ca:Mg Ratio (in Blood) | ~4:1 to 5:1 | ~6:1 to 9:1 | >10:1 |
| P:Mg Ratio (in Blood) | ~3:1 to 4:1 | ~5:1 to 7:1 | >8:1 |
| Cerebrospinal Fluid (CSF) Magnesium | >1.0 mg/dL | 0.8–1.0 mg/dL | <0.8 mg/dL |
| Note: The ratios for dietary intake are different (Ca:Mg ~7:1). Blood serum ratios are calculated from actual blood levels (mg/dL). The ratios in bone are also different (Ca:Mg ~50:1). | |||
- Notable decrease in RBC count and hemoglobin levels.
- Benzidine Test: To confirm the presence of hemoglobin (Hemoglobinuria) vs. blood (Hematuria) in urine.
- PCV (Packed Cell Volume) < 15% confirms severe anemia.
| Differential Diagnosis: Ruling Out Other Diseases | |
| Disease | Key Differentiating Symptoms |
|---|---|
| Leptospirosis | Hemoglobinuria, jaundice, high fever, abortion, anemia. |
| Bacillary Hemoglobinuria | Hemoglobinuria, jaundice, high fever; caused by Clostridium haemolyticum. |
| Anaplasmosis | Jaundice, anemia, but hemoglobinuria is absent. |
| Babesiosis | Hemoglobinuria, jaundice, presence of ticks on the body, fluctuating fever. |
| Chronic Copper Toxicity | RBC rupture and hemoglobinuria, with a history of chronic mineral imbalance. |
| 🧠 Note: Unlike infectious diseases, metabolic disorders like PPH usually present with normal or low body temperature. | |

Post Parturient Haemoglobinuria Treatment Protocols
Effective treatment for post parturient haemoglobinuria involves immediate phosphorus supplementation and supportive care.
1. Blood Transfusion for Severe Cases
If PCV < 15%, approximately 5 liters of blood can be transfused (interval: 48 hours). Follow-up fluid therapy is essential to prevent kidney damage (hemoglobinuric nephrosis).
2. Phosphorus Supplementation
- Acute Stage: 60g of Sodium Acid Phosphate in 300 ml distilled water, administered IV. Follow with SC injections every 12 hours for a total of 3 times.
- Alternative: Sodium Acid Phosphate (40.3%) — 50 ml IV, every 12 hours, maximum 3 times.
- Inj. Tonophosphan — 10–15 ml, for 2–3 days.
3. Supportive Therapy
- Dicalcium Phosphate — 100–120g, twice daily for 5 days.
- Hematinics (e.g., Iron Dextran) — during the recovery phase.
- Fluids and Electrolytes – for hydration and toxin clearance.
Prevention and Control of PPH
Prevention is always better than cure, especially for PPH in cattle.
- Ensure adequate phosphorus supply at the onset of lactation.
- Provide a balanced mineral mixture (with a balanced Ca:P ratio) regularly.
- In areas with copper deficiency, copper supplementation can help reduce the incidence of the disease.
Sample Collection for Diagnosis
Confirming a diagnosis requires specific samples:
- Urine: For color observation, Benzidine test, and confirmation of hemoglobin presence.
- Blood: For testing phosphorus, hemoglobin, RBC count, PCV, and liver/kidney function tests.
A Look at the 2014 Research on Postpartum Haemoglobinuria (PPH) by RAJUVAS University
This research was done on a serious disease occurring in buffaloes, Postpartum Haemoglobinuria (PPH). In this study, the way this disease spreads and its treatment was studied in Bikaner district of Rajasthan state and surrounding areas.
Part 1: Epidemiology – The Pattern of the Disease (Who, When, Why?)
What is the disease? PPH is a metabolic disease which occurs mostly in milking buffaloes after giving birth (parturition). In this, a severe deficiency of phosphorus occurs in the blood, due to which red blood cells (RBCs) start breaking and their hemoglobin starts coming out through urine. This is why the color of urine becomes red or like coffee.
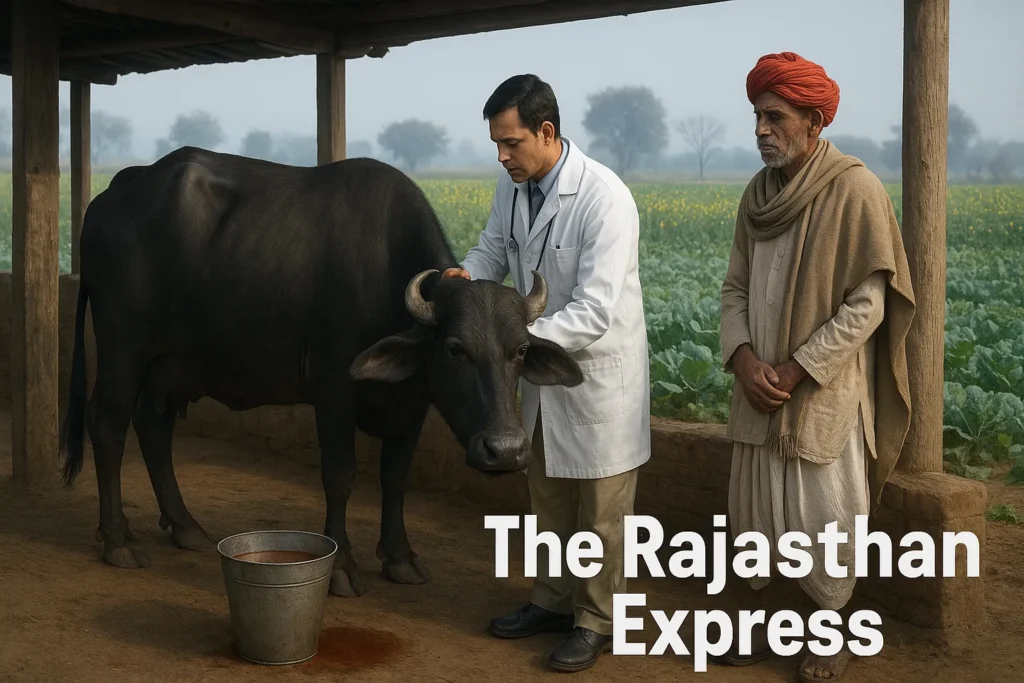
What study happened? The researchers studied 32 buffaloes suffering from PPH and treated them with a medicine called Sodium Acid Phosphate.
- Season: 87.5% of PPH cases were recorded in winter.
- Reason: Cruciferous plants (like mustard, turnip, cabbage) are grown in fields in winters, which contain an element called oxalates. This element mixes with phosphorus in the intestines and forms an insoluble compound, due to which the absorption of phosphorus does not happen. Apart from this, milk production is also at its peak in this same season, due to which the demand for phosphorus is also higher.
- Parturition Status: More than 90% of PPH cases were after parturition (Post-partum).
- Reason: There is a fixed ratio (1.3:1) of calcium and phosphorus in milk. A high production buffalo loses 30-40 grams of phosphorus daily through milk. If it is not replenished from the diet, the body goes into negative phosphorus balance, due to which hypophosphatemia occurs.
- Parity (Number of Calvings): 87.5% of cases were in buffaloes calving for the 4th to 8th time.
- Reason: Due to repeated pregnancy and milk production, the reserve of minerals in the buffalo’s body starts finishing. This reserve is still sufficient in young buffaloes (calving for the 2nd-3rd time), therefore they tolerate this deficiency.
Conclusion: The biggest victim of PPH becomes that buffalo which, in the winter season, after calving for the 4th to 8th time, is at its peak milk production and is being fed oxalate-containing fodder.
Part 2: Pathophysiology – The Root Mechanism of the Disease
This research confirms that the root cause of PPH is hypophosphatemia i.e., deficiency of phosphorus in the blood. This deficiency starts a fatal cascade:
- Decrease in ATP synthesis: Phosphorus is absolutely essential for making ATP (Adenosine Triphosphate). ATP is the “energy currency” of the cell. Deficiency of phosphorus stops the production of ATP throughout the body.
- Effect on Red Blood Cells (RBCs): Mature RBCs do not have mitochondria, therefore they depend entirely on anaerobic glycolysis for energy. This process is directly dependent on inorganic phosphate (Pi). Deficiency of Pi stops glycolysis and ATP production stops in RBCs.
- Hemolysis (Breaking of RBCs): ATP is necessary to maintain the flexibility and integrity of the RBC membrane. Without ATP, RBCs become hard and brittle. When these delicate cells pass through narrow blood capillaries, they break easily. This is called intravascular hemolysis.
- Hemoglobinuria: The hemoglobin freed from the broken RBCs dissolves in the blood plasma. When this hemoglobin filters through the kidneys and reaches the urine, the color of urine becomes red, brown, or coffee-like.
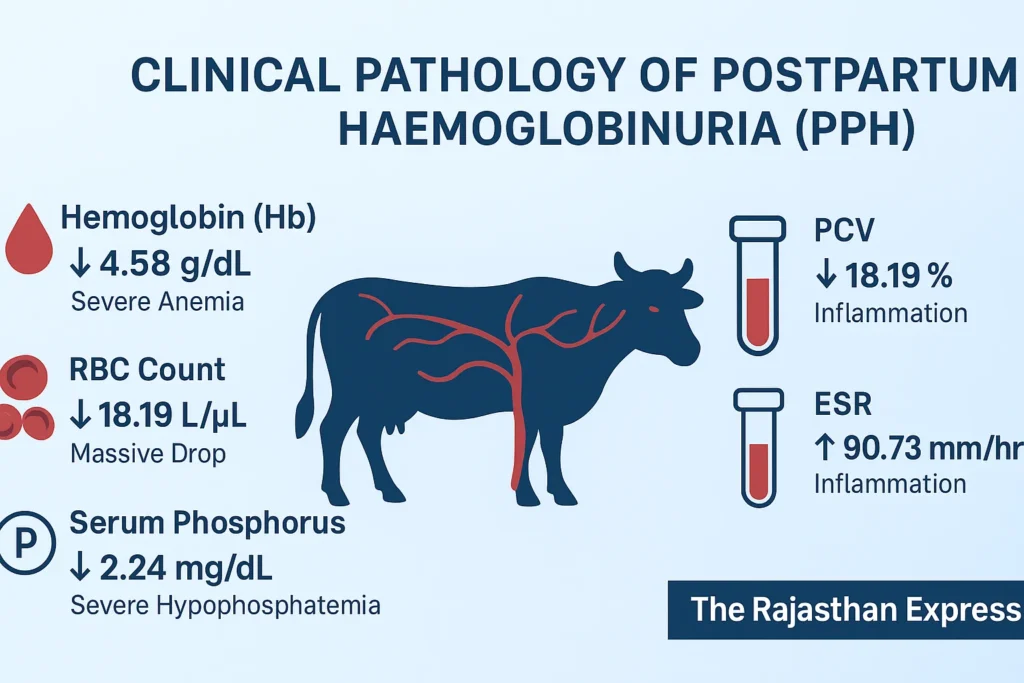
Part 3: Clinical Pathology – The Results of the Blood Test
The data of the hematological parameters given in the report confirm the above mechanism:
| Hematological Changes in Buffaloes Afflicted with PPH | |||
| Parameter | Observed Value | Normal Range | Remarks |
|---|---|---|---|
| Hemoglobin (Hb) | 4.58 g/dL | 8 – 12 g/dL | Clear indication of severe anemia. |
| RBC Count | 18.19 Lakh/µL | 50 – 70 Lakh/µL | Massive drop in the number of red blood cells. |
| PCV / Hematocrit (Hct) | 18.19% | 24 – 46% | Only 18% of blood is red cells, confirming anemia. |
| ESR | 90.73 mm/1st hr | 0 – 15 mm/1st hr | Extremely high, indicates severe inflammation and anemia. |
| Serum Phosphorus | 2.24 mg/dL | 4 – 8 mg/dL | Severe hypophosphatemia → Key diagnostic marker of PPH. |
| Summary: This table clearly shows that PPH starts with severe phosphorus deficiency in the blood, which leads to hemolysis (RBC rupture) and severe anemia. 👉 The combination of low phosphorus + anemia is the hallmark of PPH diagnosis. | |||
Part 4: Rationale of Treatment (The Logic of the Treatment)
There is a clear scientific logic behind the treatment protocol adopted in this study:
- Sodium Acid Phosphate: This is the etiological treatment, meaning it removes the root cause (phosphorus deficiency). Its level is increased immediately in the blood by giving IV, and its effect is maintained for a long time by giving SC/oral.
- Ascorbic Acid (Vitamin C): This is a powerful antioxidant. Oxidative stress increases greatly during hemolysis, which damages RBCs further. Vitamin C reduces this oxidative stress and protects RBCs from further breaking.
- Botropase: Blood clotting ability can be affected due to widespread hemolysis and micro-bleeding can occur. Botropase (which is derived from a snake venom) works as a hemostatic agent and helps in controlling bleeding.
- Combination of Vitamin A, D, E:
- Vitamin D: Helps in regulating the absorption and metabolism of calcium and phosphorus.
- Vitamin E: Another antioxidant like Vitamin C, which helps in stabilizing the membrane of RBCs.
- Vitamin A: Assists in overall immunity and recovery.
Part 5: Overall Conclusion and Modern Outlook
- This research underlines that PPH is not just a symptom, but a complex metabolic crisis.
- The 60% success rate tells that this protocol is effective, but it is not 100%. This might be because in very advanced cases, organ damage (especially kidney damage) has become irreversible.
- In modern management, combined injections of calcium and phosphorus (like calcium phosphorus borogluconate) are considered more effective for its treatment, because often hypocalcemia (calcium deficiency) is also present simultaneously.
- The most important thing is prevention: It is mandatory to give phosphorus-containing mineral mixture to high production buffaloes, especially after parturition. Also, control should be kept on the excessive consumption of oxalate-containing fodder (like mustard).
Main Role:
This research was conducted by a team of researchers from the Department of Teaching Veterinary Clinical Complex, Rajasthan University of Veterinary and Animal Sciences (RAJUVAS), Bikaner.
🔬 Research Team Members:
- Mrs. Sanjhali Soren (Ms. Sanjhali Soren) (Principal Researcher)
- Dr. Mukesh Srivastava (Dr. Mukesh Srivastava) (Assistant Professor and Corresponding Author) E-mail: drmukeshvetmed@rediffmail.com
- Dr. J.P. Kachhawa (Dr. J.P. Kachhawa) (Research Guide)
- Mrs. Punam Soren (Ms. Punam Soren) (Research Associate)
- Mrs. Anuradha Kumari (Ms. Anuradha Kumari) (Research Associate)
- Mrs. Ankita Sharma (Ms. Ankita Sharma) (Research Associate)
🏛️ Institutional Affiliation:
Rajasthan University of Veterinary and Animal Sciences (RAJUVAS)
Location: Bikaner, Rajasthan – 334001
Department: Department of Teaching Veterinary Clinical Complex
📄 Research Publication Details:
- Research Title: “Clinical Studies on Postparturient Haemoglobinuria in Buffaloes”
- Publication: Intas Polivet Journal
- Year: 2014
- Volume: 15 (II)
- Pages: 518-522
A comprehensive guide to Post Parturient Haemoglobinuria (PPH) in cattle. Learn the main causes of phosphorus deficiency, its critical link to milk fever, symptoms, and advanced treatment protocols for this metabolic disorder.
THE RAJASTHAN EXPRESS