Understanding Pregnancy Toxemia (Pregnancy Ketosis) in Ewes and Does
Definition and Etiology
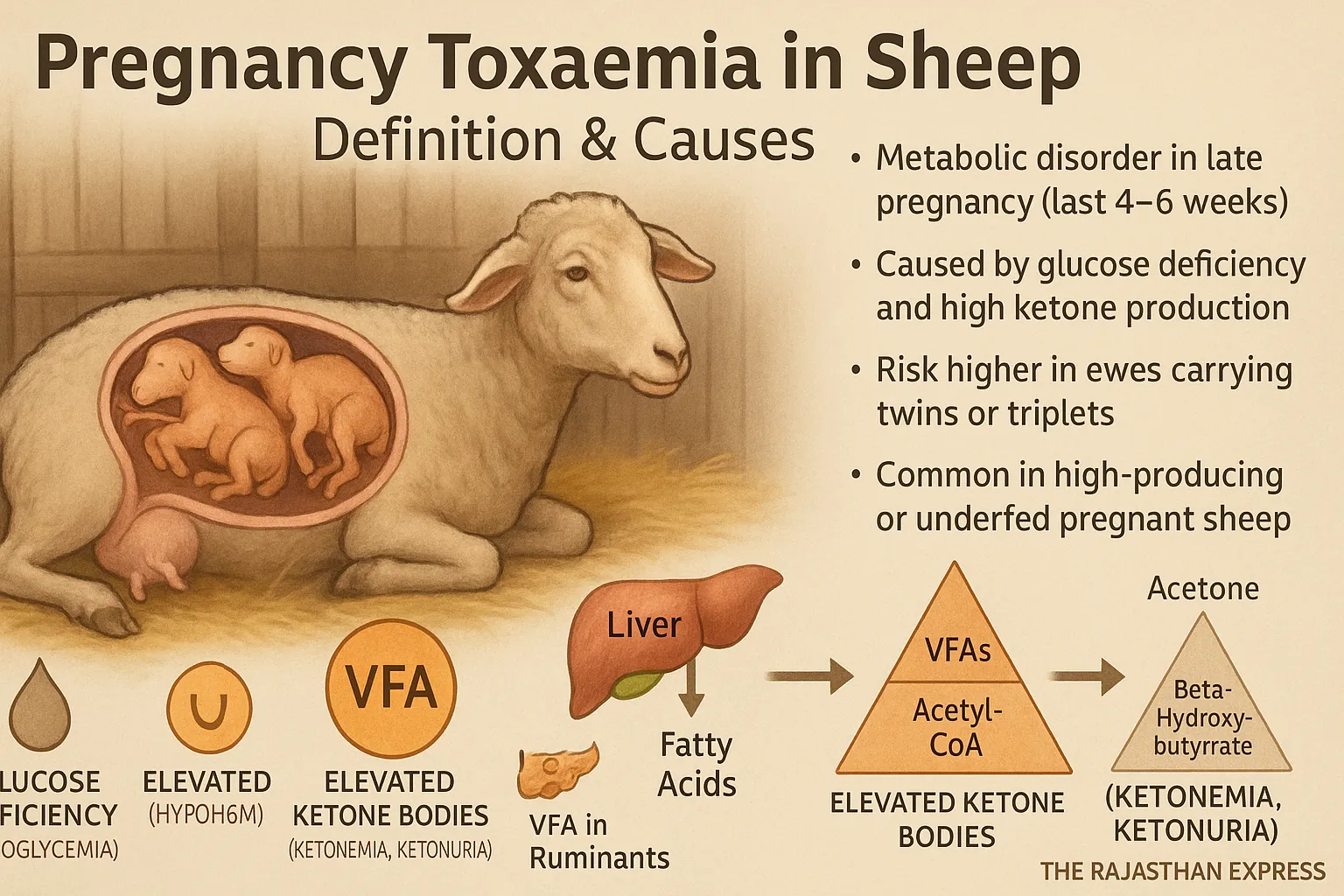
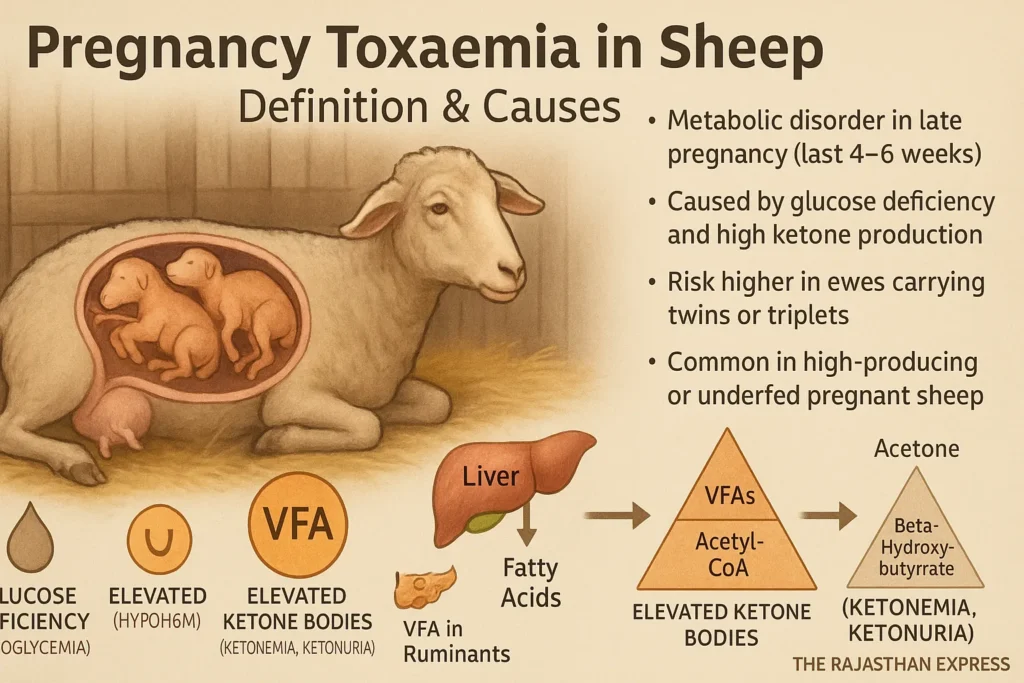
Pregnancy Toxemia is a significant metabolic disease occurring in pregnant sheep. It is also called Pregnancy Ketosis in sheep. The main causes of this disease are low blood glucose (hypoglycemia) and an excessive increase in ketone bodies (ketosis). It is a nutritional metabolic disorder that arises in the last stage of pregnancy (last 4-6 weeks) due to a disruption in the metabolism of carbohydrates and fatty acids.
The prevalence of this disease is approximately 5% to 20%. If left untreated, the mortality rate can reach up to 80%. Even with intensive treatment, about 40% of sheep die. Furthermore, this disease can also cause abortion, dead fetuses, acute toxicity, and maternal death, especially when the fetus dies in the uterus.
Pregnancy is a stage where the sheep requires adequate nutrition to meet its body’s metabolic needs and ensure fetal development. Fat accumulation before pregnancy is important to meet the energy demands of the fetus’s rapid growth and subsequent milk production. However, towards the end of pregnancy, the sheep’s appetite decreases, leading the animal into a state of negative energy balance. This can impact fundamental cellular processes.
The Ketosis Process: When there is a glucose deficiency in the body, the beta-oxidation of stored fat begins. In this process, fatty acids break down into Acetyl-CoA. A portion of this Acetyl-CoA enters the Krebs cycle to produce energy (ATP), while the excess Acetyl-CoA is converted into ketone bodies (mainly beta-hydroxybutyrate, acetoacetate, and acetone) in the liver. An increase in ketone bodies in the blood is called ketonemia, and their presence in urine is called ketonuria.
Pregnancy Toxemia (Pregnancy Ketosis) in Ewes and Does
| Also Known As | Pregnancy Disease, Lambing/Kidding Sickness, Twin Lamb/Kid Disease |
|---|---|
| Definition | A severe metabolic disorder in late gestation (last 4–6 weeks) of sheep and goats, caused by hypoglycemia and ketonemia due to Negative Energy Balance (NEB), leading to impaired carbohydrate and fat metabolism. |
| Etiology & Pathophysiology |
|
| Risk Factors |
|
| Clinical Presentations |
|
| Diagnosis |
|
| Differential Diagnoses |
|
| Treatment |
|
| Prevention & Management |
|
| Prognosis | Guarded to poor. Mortality up to 80% if untreated; intensive treatment still results in ~40% deaths. Earlier intervention improves survival. |
| Regulatory & Welfare Considerations | Recognized as a major animal welfare concern in sheep/goat production. Prevention through nutritional management is emphasized in extension guidelines (USDA, FAO, OIE). Severely affected non-ambulatory animals may require humane euthanasia per welfare codes. |
| Sources: Merck Veterinary Manual; FAO Sheep Nutrition Guidelines; USDA Extension Services; OIE Animal Welfare Standards; The Rajasthan Express | |
This disease specifically arises when there is a sudden or sharp decline in nutritional levels during the final 4–6 weeks of pregnancy. When the pregnant sheep does not receive sufficient energy (in the form of carbohydrates), the body’s energy supply becomes inadequate. In non-ruminant animals, the final digestive product of carbohydrates is glucose, but in ruminant animals (such as sheep, goats, cows, buffaloes, camels, etc.), most carbohydrates are fermented by microbes in the rumen into Volatile Fatty Acids (VFAs). Ruminant animals obtain nearly 70% of their energy from these VFAs. This disease is most common in sheep with twins or triplets because it becomes difficult to meet the excessive energy demand generated by fetal growth.
Metabolic Disease in Animals: Definition, Types, and Key Characteristics
Definition:
Metabolic Diseases are those diseases which occur due to deficiency, imbalance of nutrients, or disturbance of metabolism in the body. These diseases are especially related to milk production, pregnancy, and the energy requirements of the body.
Read More About : Metabolic Disease
Main Features of Metabolic Disease in Dairy Cattle
- These diseases are Non-Contagious — do not spread from one animal to another.
- In most cases, these diseases are related to the production system, hence they are also called Production Diseases.
- Especially pregnant and milk-producing animals (like cow and buffalo) are more susceptible to these diseases.
- The possibility of metabolic diseases increases with increasing milk production.
- In native cows (Zebu cattle), the highest possibility of metabolic disease is found in the third calving.
- In exotic cows (Exotic Cattle), this possibility is highest in the fifth calving.
- In buffaloes, the possibility of metabolic diseases is mostly in the fourth calving.
- The order of possibility of metabolic diseases is as follows:
Exotic Cow > Native Cow > Buffalo - The possibility of Downer Cow Syndrome, Ketosis, Postpartum Haemoglobinuria, and Mastitis disease is higher in exotic cows, especially in the Holstein-Friesian breed.
- These same diseases are found mostly in the Sahiwal breed in native cows.
- The possibility of Milk Fever is highest in Jersey cows.
We have also explained these diseases in detail.
Explore the key metabolic diseases in cattle with quick links to each section:
- Milk Fever – Calcium deficiency immediately after calving
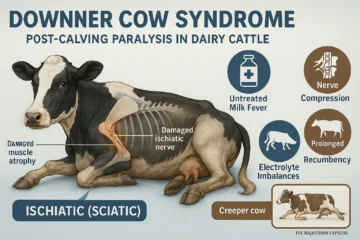
- Downer Cow Syndrome – Complications from prolonged lying after milk fever
- Ketosis In Cattle – Energy deficiency and ketone accumulation
- Postparturient Haemoglobinuria – Red blood cell destruction due to phosphorus deficiency
- Grass Tetany – Muscle cramps from magnesium deficiency
- Pregnancy Toxemia – Energy deficiency in late pregnancy
Adverse Effects of Excess Ketone Bodies
- Ketonemia: An increase in the concentration of ketone bodies (mainly beta-hydroxybutyrate) in the blood.
- Ketonuria: The presence of ketone bodies in the urine.
Disease Terminology and Root Cause
- In cows and buffaloes, this condition is called Ketosis.
- In sheep and goats, especially at the end of pregnancy, it is called Pregnancy Toxemia or Pregnancy Ketosis.
- Other Names: In sheep and goats, it is also called Pregnancy Disease, Lambing/Kidding Sickness, and Twin Lamb/Kid Disease.
- Main Biochemical Cause: Low blood glucose (Hypoglycemia).
- Root Cause: Negative Energy Balance (NEB)
Ketosis and Pregnancy Toxemia are primarily caused by Negative Energy Balance (NEB). In the NEB condition, energy expenditure exceeds energy intake. This results in hypoglycemia, ketonemia, and ketonuria. This state develops due to a severe disruption in fat and carbohydrate metabolism.
Seasonal Influence: During summers or droughts, when animals receive low-quality and/or insufficient fodder, the breakdown of stored body fat (lipolysis) increases. This increases the production of ketone bodies, which accumulate in the blood (ketonemia) and are excreted through urine (ketonuria).
Major Causes of Ketosis and Pregnancy Toxemia
Primary Causes of Pregnancy Toxaemia in Ewes
1. Nutritional Causes
- Loss of appetite or fasting (Inappetence or Fasting)
- Low energy-dense diet (especially deficiency of carbohydrates/glucose precursors)
- Excessive Protein Intake:
- Explanation: Protein is not stored in the body in large quantities like carbohydrates or fat. When excess protein is consumed, it is broken down into amino acids.
- Unused amino acids have their nitrogen converted into urea by the liver and excreted in urine through the kidneys. This process consumes energy.
- The primary function of protein is to build and repair tissues, not to provide energy.
- Using protein for energy (gluconeogenesis) is a slow and less efficient process.
- Conclusion: Especially during high energy-demand states like pregnancy or lactation, a diet based solely on or rich in protein but low in energy increases the risk of ketosis. Therefore, a balanced diet with a proper ratio of carbohydrates, fats, and protein is essential.
2. Roughage-Concentrate Imbalance
- The ideal roughage:concentrate ratio in the diet for ruminant animals (cow, buffalo, sheep, goat) is approximately 65:35 (⅔ roughage : ⅓ concentrate).
- Effect of Imbalance: If this ratio is disturbed (e.g., too much roughage and too little concentrate), the possibility of ketosis/pregnancy toxemia increases.
- ➤ Imbalance of VFAs (Volatile Fatty Acids):
- On a balanced diet, the normal ratio of VFAs produced in the rumen is:
- Acetate : Propionate : Butyrate ≈ 7 : 2 : 1
- This means:
- Ketogenic VFA (Acetate + Butyrate) : Glucogenic VFA (Propionate) ≈ 4 : 1
- On a balanced diet, the normal ratio of VFAs produced in the rumen is:
- Explanation:
- Propionate is converted into glucose in the liver, hence it is called a glucogenic VFA.
- Acetate and Butyrate promote the formation of ketone bodies, hence they are called ketogenic VFAs.
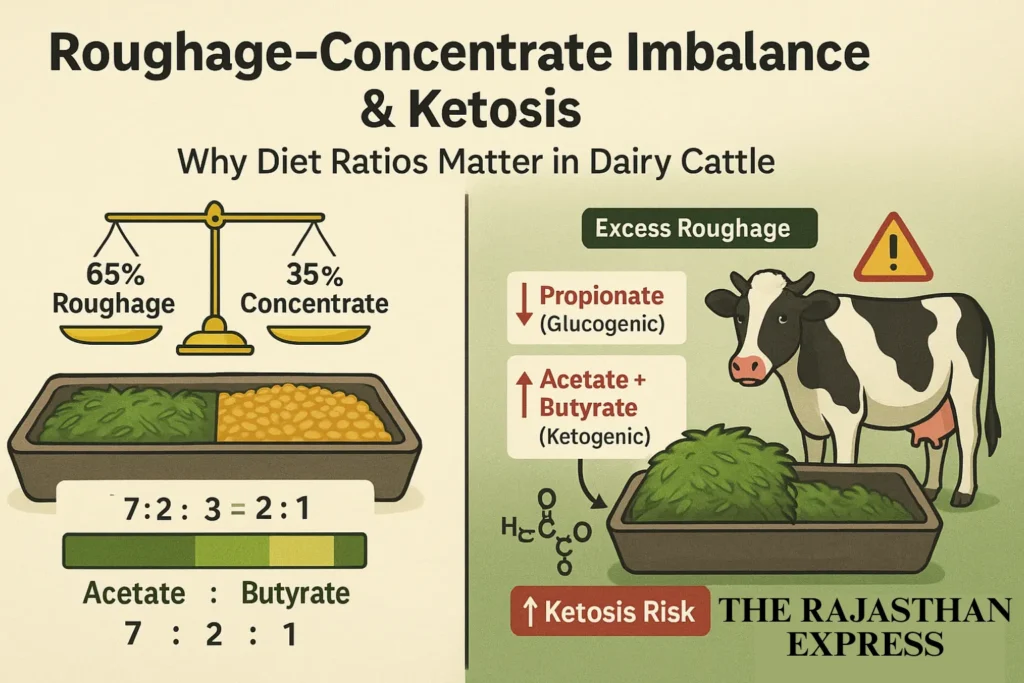
- Consequence: If an excessive amount of roughage (low concentrate) is given in the diet, the production of propionate in the rumen decreases and the ratio of ketogenic VFAs (acetate, butyrate) increases. This causes the level of ketone bodies in the blood to rise, which can result in ketosis or pregnancy toxemia.
- Summary: A higher amount of roughage and a lower amount of concentrate in the total diet (disruption of the 65:35 ratio) leads to a deficiency of propionate and an excess of ketogenic VFAs, which are major risk factors for ketosis/pregnancy toxemia.
3. Animal-Related Causes
- High Milk Yield: In high-yielding dairy animals, a large amount of lactose (milk sugar, approximately 45-50 grams per kilogram of milk) is lost with the milk. This lactose is made from glucose, which can lead to energy deficiency (NEB) and put extra strain on the liver.
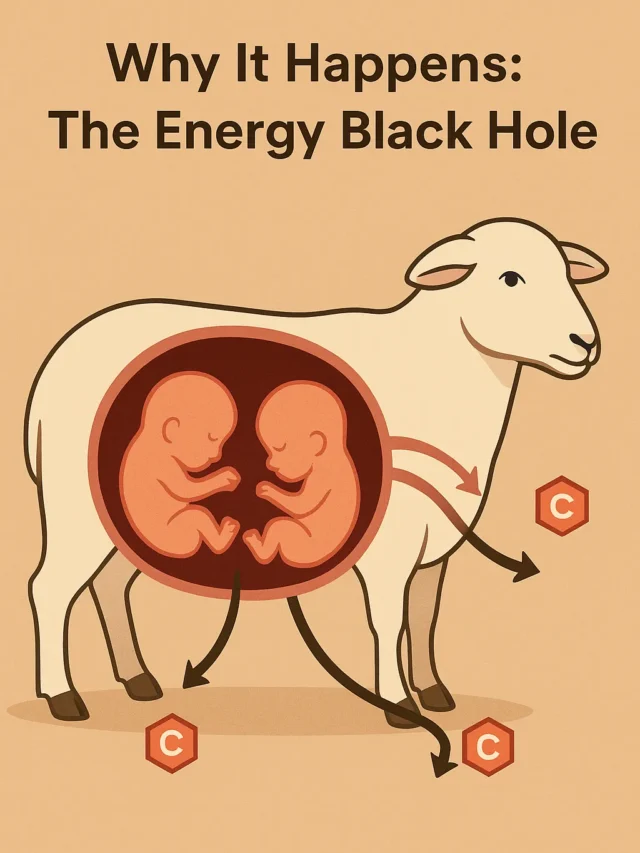
- Multiple Fetuses: In sheep/goats with twins or triplets, the energy demand for fetal growth is very high and often cannot be met.
- Obesity: Excessive obesity can cause Insulin Resistance, which reduces the entry of glucose into cells and increases the breakdown of fat (which produces ketone bodies).
- Parasitic Infestation: Severe blood-sucking worm infestations like Haemonchus contortus cause anemia and weakness, which can promote NEB by reducing appetite.
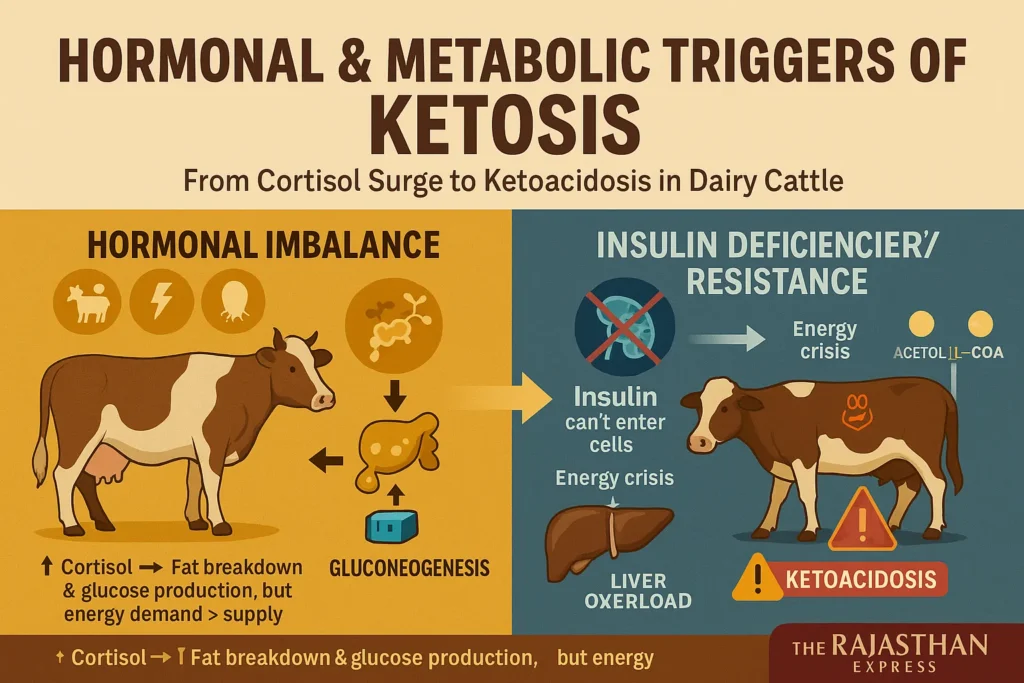
4. Hormonal & Metabolic Causes
- Hormonal Imbalance: During pregnancy, parturition, or other stress, increased levels of glucocorticoid hormones like cortisol can enhance fat breakdown and gluconeogenesis, but this is often insufficient to meet energy demands. In some cases, the capacity for gluconeogenesis may be limited.
- Insulin Deficiency or Resistance (Less Common Cause):
- If there is a deficiency of the insulin hormone in the body or if cells become resistant to insulin, then the glucose present in the blood cannot effectively enter the cells.
- This results in:
- Potential increase in blood glucose levels (hyperglycemia).
- A deficiency of glucose in the cells (cellular energy crisis).
- Due to this energy crisis, the body begins to break down stored fat (triacylglycerol) and glycogen.
- Beta-oxidation of fatty acids occurs, producing Acetyl-CoA.
- An excess of Acetyl-CoA in the liver increases the production of ketone bodies (acetoacetate, beta-hydroxybutyrate, acetone).
- An excessive amount of ketone bodies can cause blood acidity (metabolic acidosis), which is called Ketoacidosis. This severely disrupts the acid-base balance.
- 5. Impaired Carbohydrate Metabolism: This is a combined result of NEB and the causes described above.
Diagnostic Indicators and Clinical Signs of Ovine Pregnancy Toxemia
Recognizing the Symptoms of Pregnancy Toxemia
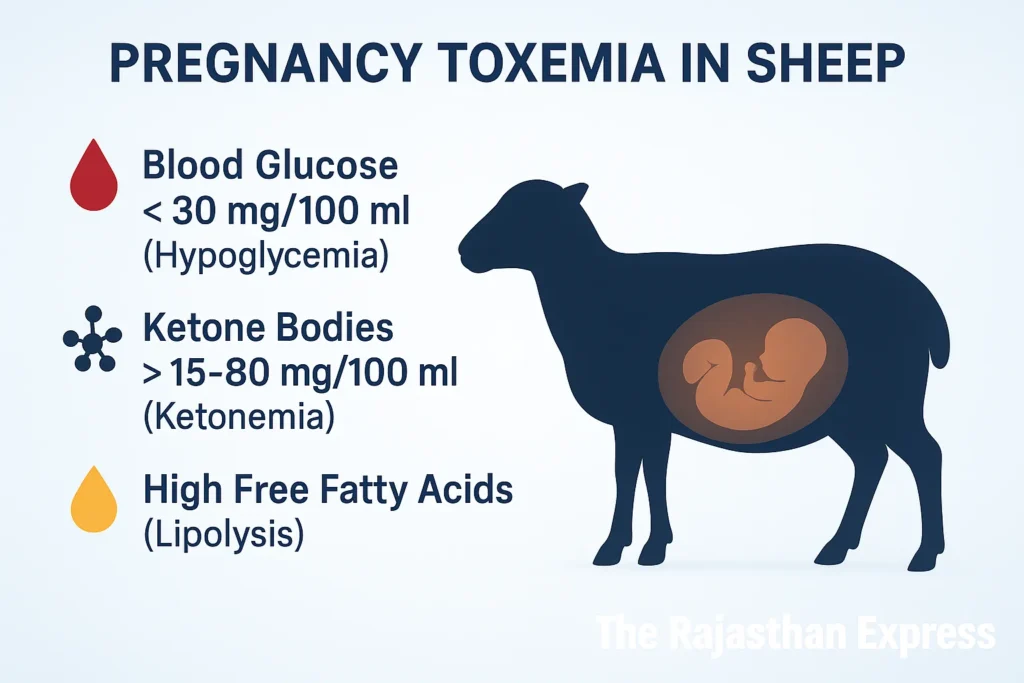
Diagnostic Indicators
- In the early stage:
- Blood Glucose: < 30 mg/100 ml (Normal: 40–60 mg/100 ml) – Hypoglycemia
- Ketone Bodies (Blood): > 15 mg/100 ml, sometimes up to 80 mg/100 ml (Normal: 1–4 mg/100 ml) – Ketonemia
- Free Fatty Acids (FFAs): The level of FFAs in the blood increases, indicating fat breakdown (lipolysis).
A realistic scene of a vet diagnosing a downer ewe. Learn the steps for on-farm assessment of Pregnancy Toxemia and why immediate veterinary intervention is critical for survival.
| Ketone Body Parameters in Ruminant Metabolic Disorders | |||
| Parameter | Normal Level | Moderate Elevation | Severe Ketosis |
|---|---|---|---|
| Blood Ketones | 1–4 mg/100 mL | 5–15 mg/100 mL | >15 mg/100 mL (up to 80+ mg/100 mL) |
| Clinical Correlation | Normal metabolic state | Subclinical ketosis | Clinical pregnancy toxemia / ketosis |
| Primary Ketone Form | β-hydroxybutyrate (BHB) | β-hydroxybutyrate (BHB) | β-hydroxybutyrate (BHB) + acetoacetate |
| Elevated blood ketones indicate progression from normal metabolism → subclinical ketosis → severe clinical ketosis/pregnancy toxemia. | |||
| Normal Blood Glucose Ranges in Ruminants | |||
| Species | Normal Range (mg/dL) | Hypoglycemic Threshold (mg/dL) | Critical Low Value (mg/dL) |
|---|---|---|---|
| Sheep | 44–81 | <40 | <30 |
| Goats | 48–76 | <45 | <35 |
| Cattle | 42–75 | <40 | <30 |
|
🟢 Normal range → Healthy metabolic state 🟡 Hypoglycemic threshold → Risk of subclinical hypoglycemia 🔴 Critical low value → Severe metabolic disorder, emergency intervention needed | |||
Predisposing Factors
- Lack of energy-rich diet (carbohydrate/glucose sources).
- Management-related stress: Crushing, shearing, transportation, sudden environmental changes.
- Drenching (dosing medicine) or other stressful interventions during the second half of pregnancy.
- Excessive obesity (promotes insulin resistance).
- Severe worm infestations like Haemonchus contortus causing anemia and weakness.
- Twins or triplets (massive increase in the mother’s energy demand).
Clinical Signs of Pregnancy Toxemia
The symptoms of Pregnancy Toxemia and dairy ketosis are similar. In sheep/goats, symptoms usually start 1-3 weeks before parturition.
- Early Signs:
- Lethargy, apathy (Depression)
- Reduced or complete loss of interest in eating and drinking (Anorexia)
- Separation from the herd
- Weight loss
- Signs of dehydration (dry skin, sunken eyes)
- Constipation
- “Hangdog appearance” – Standing tired with head down, back hunched.
- Teeth grinding (Bruxism)
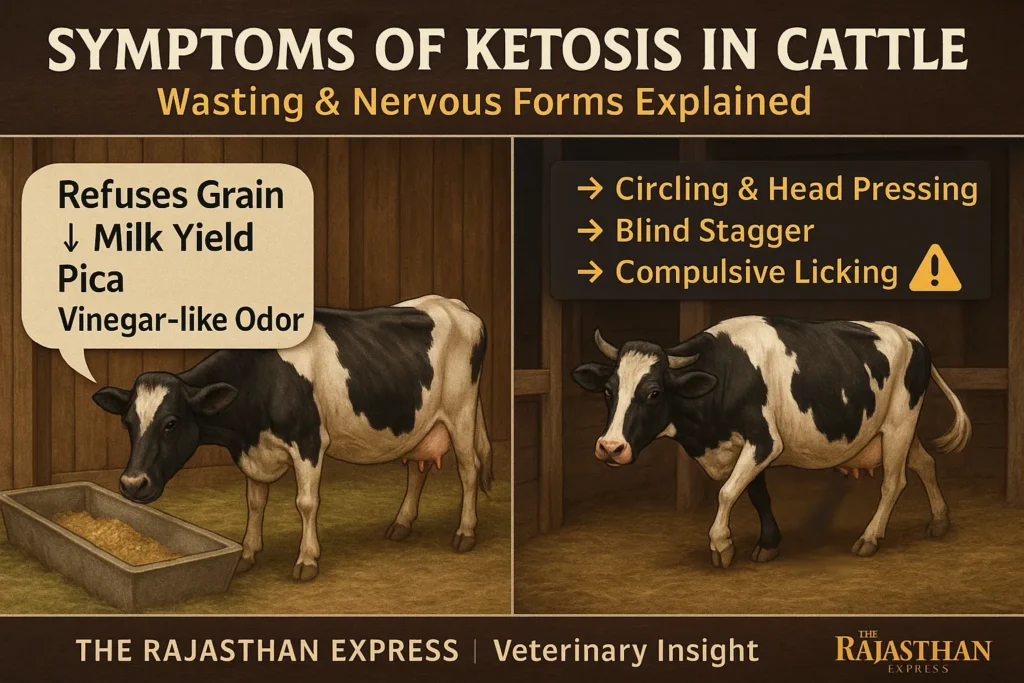
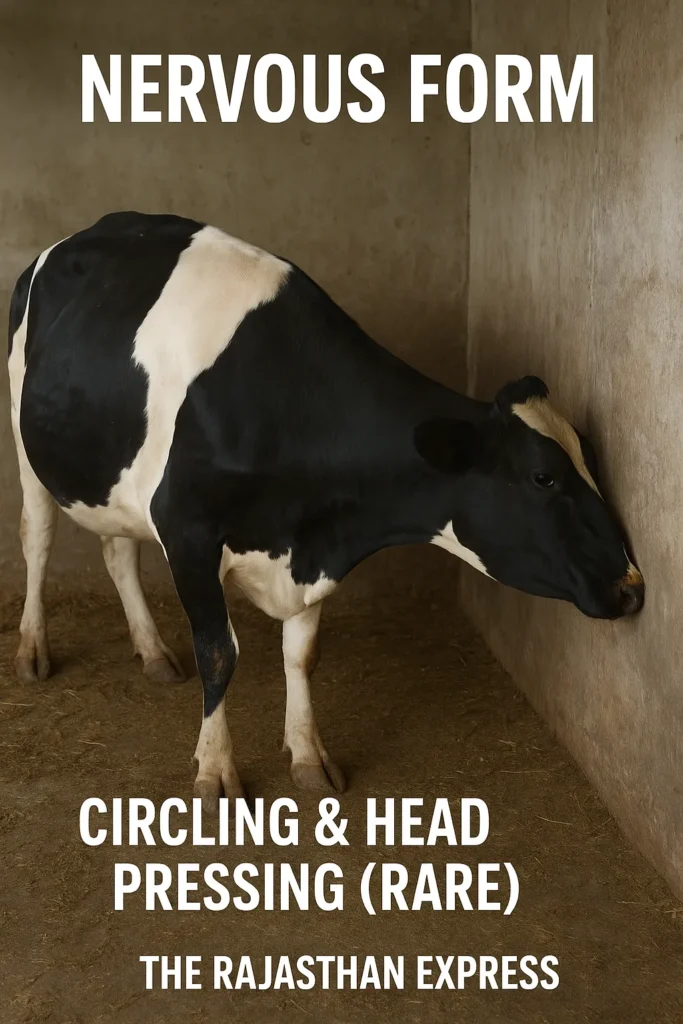
- Neurological Signs (Indicate Progression):
- Pressing or banging head against walls or objects (Head pressing)
- Blindness-like behavior (not understanding direction, bumping into things)
- Posture of looking upwards at the sky (Star gazing)
- Muscle tremors (muscle twitching), especially around the head and lips
- Lip smacking
- Head tilted to one side (Head tilt)
- Staggering walk, lack of balance (Ataxia)
- Circling – Sheep/goats often circle with legs crossed.
- Convulsions
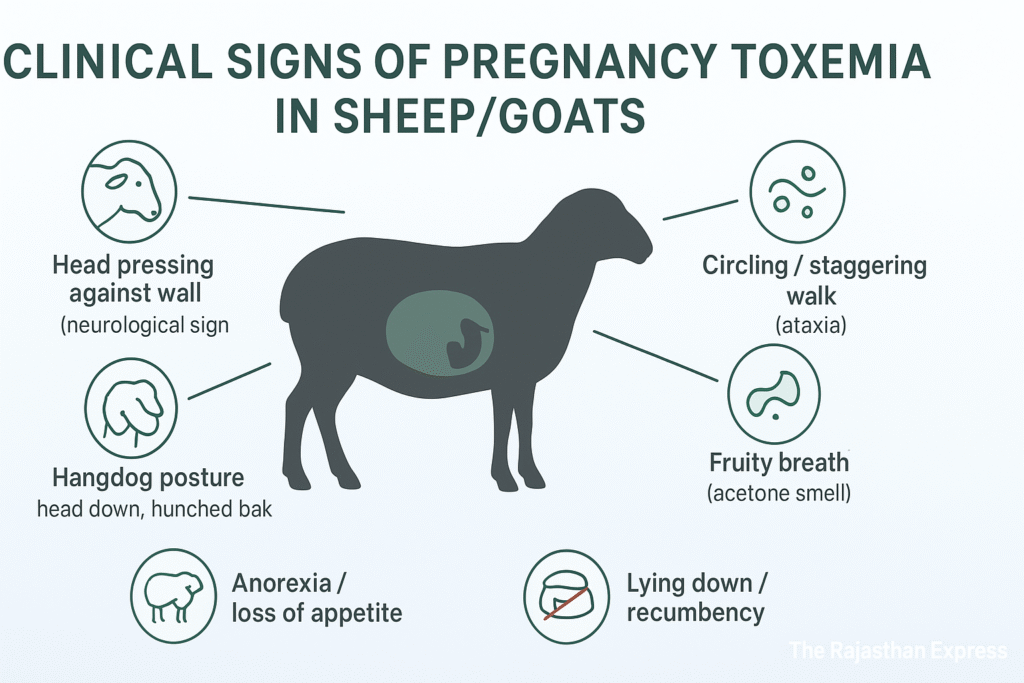
- Other Specific Signs:
- A fruity or vinegar-like smell from breath, urine, and milk: This is due to acetone and is a key clinical sign of ketonemia/ketonuria.
- Difficulty in birthing (Dystocia): Affected sheep/goats have difficulty with normal parturition.
- Late Stage:
- Lying down (Recumbency)
- Coma
Outcome: Without treatment, death occurs within 2-10 days in 80% of cases. The animal often goes into a state of Shock.
Diagnosis and Treatment of Pregnancy Toxemia in Sheep and Goats
How to Diagnose Pregnancy Toxaemia in Ewes and Does
1. Clinical History and Signs
- Final stage of pregnancy (especially sheep/goats with twins/triplets).
- Specific clinical signs: Lethargy, loss of appetite, weight loss, dehydration, neurological symptoms (head pressing, blindness, circling, convulsions), fruity/vinegar-like smell in breath/urine/milk (acetone), hangdog appearance.

2. Physical Examination
A ketotic smell on the breath is an early indicator.
3. Laboratory Diagnosis
- Blood Glucose: Hypoglycemia (< 30 mg/dL; Normal: 40-60 mg/dL . Sheep: 44-81, Goats: 48-76, Cattle: 42-75 mg/dL).
| Normal Blood Glucose Ranges in Ruminants | |||
| Species | Normal Range (mg/dL) | Hypoglycemic Threshold (mg/dL) | Critical Low Value (mg/dL) |
|---|---|---|---|
| Sheep | 44–81 | <40 | <30 |
| Goats | 48–76 | <45 | <35 |
| Cattle | 42–75 | <40 | <30 |
|
🟢 Normal range → Healthy metabolic state 🟡 Hypoglycemic threshold → Risk of subclinical hypoglycemia 🔴 Critical low value → Severe metabolic disorder, emergency intervention needed | |||
- Ketone Bodies:
- Blood (Ketonemia): Serum β-hydroxybutyrate (BHB) > 3.0 mmol/L (≈ 3,000 µmol/L) (the most reliable biomarker for diagnosis). In the early stage, > 1.0-1.4 mmol/L is also concerning.
- Urine (Ketonuria): Rothera’s Test positive (common kit for rapid check of ketone bodies in urine).
- Plasma Cortisol: > 10 ng/mL (indicator of stress/metabolic crisis, not specific for diagnosis).
- Acid-Base Status: Metabolic acidosis (ketoacidosis) in the advanced stage.
- Advanced Complications: Liver damage (reduced liver function), kidney failure, severe dehydration (water deficiency).
Differential Diagnosis and Treatment for Goat Toxemia
Differential Diagnosis (Other diseases with similar symptoms)
- Hypocalcemia (Milk fever): Occurs at the end of pregnancy/parturition. Distinct neurological symptoms, weakness, recumbency. Low blood calcium (< 7-8 mg/dL).
- Listeriosis: Unilateral facial paralysis, circling, convulsions. Confirmed by cerebrospinal fluid (CSF) testing.
- Cerebral Abscess: Slowly progressive neurological symptoms, may have fever.
- Other Acidosis Causes: Grain overload, kidney failure.
- Uterine Torsion: Inability to give birth, abdominal pain.
- Infectious Abortion: From Brucella, Chlamydia, etc. Usually involves fever.
- Rabies: Very rare, hydrophobia, paralysis, aggression. Ultimately fatal. (Note: Symptoms may be somewhat similar, but it is very rarely a differential for pregnancy toxemia).
Pregnancy Toxemia Treatment Protocols
(Guidelines; a veterinarian should treat according to the individual animal’s condition)
- Immediate Energy Correction:
- IV Glucose: 50-100 ml of 50% Dextrose as a slow IV Fluid Therapy. Can be repeated at 4-6 hour intervals as needed.
- Oral Glucose Precursors:
- Propylene Glycol: Most effective. 60 ml orally, every 12 hours, for 3-5 days. Converted to glucose in the liver.
- Glycerol: Alternative. ~110 grams (approx. 90-100 ml) orally, daily.
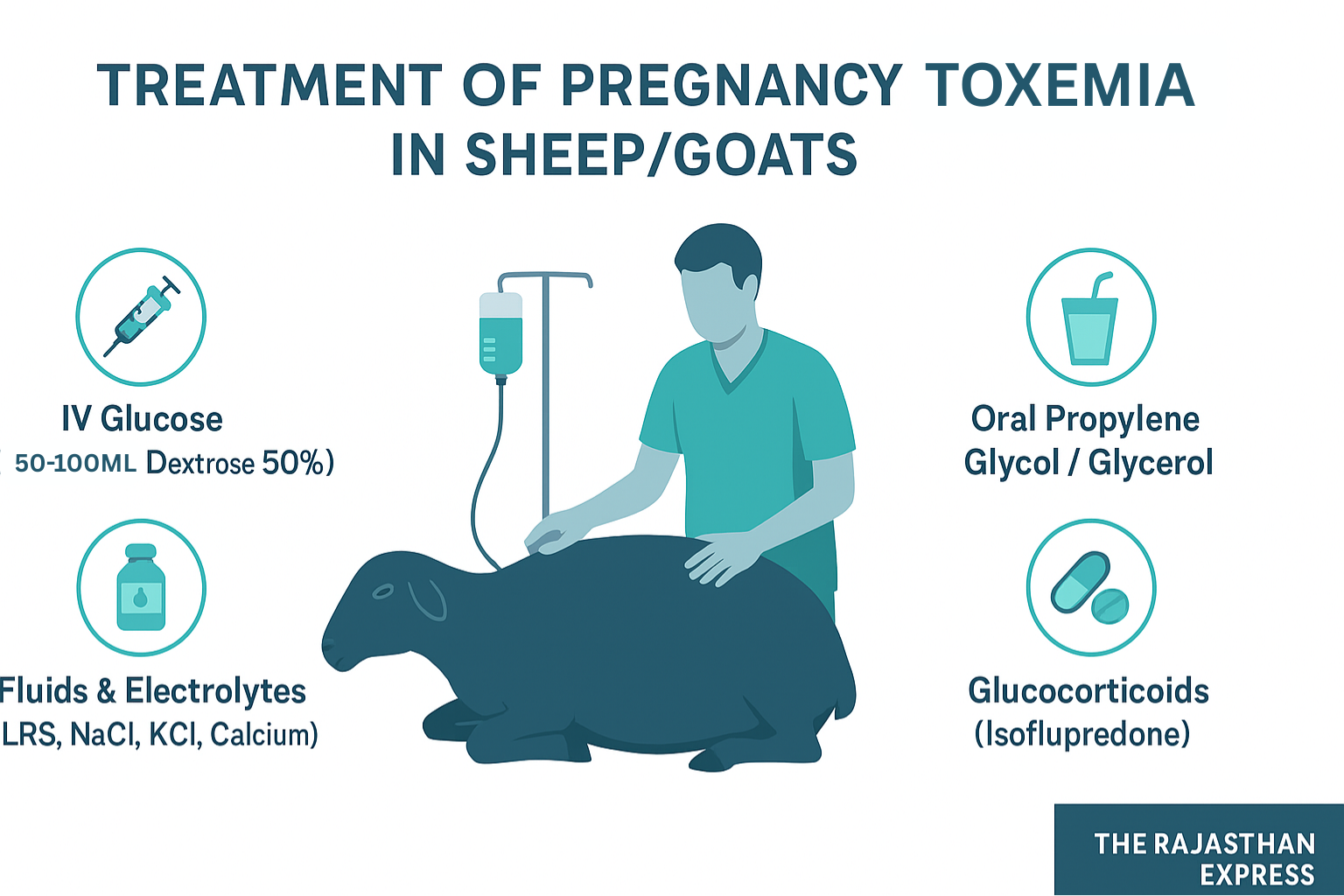
- Fluid & Electrolyte Therapy:
- Correction of dehydration and acidosis is essential.
- IV/SC: Lactated Ringer’s Solution (LRS) or 0.9% Sodium Chloride. Volume and frequency depend on severity of dehydration (3-4 liters every 6-12 hours IV in severe cases, SC in less severe). Potassium (KCl) and Calcium (calcium borogluconate) are often added to the solution.
- Other Therapeutic Options:
- Insulin: Protamine Zinc Insulin (PZI): 20-40 units (or 0.4-0.6 U/kg), Subcutaneous (SC), every 24-48 hours. Increases glucose utilization by cells. Blood sugar monitoring is necessary.
- Glucocorticoids: Isoflupredone: 10-20 mg (or 0.1-0.2 mg/kg), Intramuscular (IM), once. Stimulates gluconeogenesis and aids stress response. Caution: May cause abortion.
Severe Cases and Life-Saving Measures
- Surgery (Caesarean Section): If the animal is critically ill and the fetuses are alive/developed, an immediate C-section is the best way to save the mother’s life and save the lambs/kids. It immediately eliminates the massive energy demand.
Prevention and Control of Ovine Pregnancy Toxemia
Late Gestation Nutritional Management (KEY)
- Steaming Up Ration: In the last 6-8 weeks of pregnancy (last trimester), an additional 200-300 (Avg. – 250Gm) grams of energy-dense concentrate (grain-based) should be provided on top of the main maintenance ration. This meets the energy needs for the fetuses’ rapid growth and preparation for milk production.
- Diet Balance: Provide a balanced diet with high energy density. Aim for 10-12% Crude Protein (CP) and sufficient easily digestible carbohydrates (TDN > 55-60%). Avoid grain overload – increase gradually.
- Body Condition Score (BCS): Maintain optimal BSC during breeding and pregnancy (sheep: 3.0-3.5, goat: 3.0). Both excessive obesity and weakness increase risk.
Body Condition Score (BCS): A Vital Tool for Livestock Health and Metabolic Disease Prevention
Body Condition Score (BCS) is a standardized method used in animal husbandry and veterinary medicine to assess the fat (adipose tissue) reserves in an animal’s body. It is based on a visual and tactile (checked by touch) technique.
Its purpose is not only to determine if an animal is lean or fat but to understand its Energy Balance status—that is, whether the animal’s body has an energy deficiency or not. This balance directly affects its overall health, production and reproductive capacity, and the risk of metabolic diseases. Specifically, BCS plays a key role in the diagnosis of diseases like Ketosis and Pregnancy Toxemia, which arise from an energy deficiency in the body.
| BCS Scales and Physical Condition Descriptions | ||
| BCS (1–5 Scale) | BCS (1–9 Scale) | Description of Physical Condition |
|---|---|---|
| 1 | 1–2 | Very Lean (Emaciated): Bones (hips, back, ribs) are clearly visible and very prominent. No fat can be felt. Severe muscle loss. |
| 2 | 3–4 | Lean (Thin): Bones are easily visible and palpable. Slight muscle present, but fat covering is negligible. |
| 3 | 5–7 | Ideal: Bones not visible but can be easily felt. Smooth, rounded back and hips. Balanced muscle and fat coverage. |
| 4 | 8 | Fat: Bones are difficult to feel due to thick fat covering. Hips appear wide and flat. Risk of over-conditioning. |
| 5 | 9 | Obese: Bones almost impossible to feel. Excess fat around neck, hips, and tailhead. Reduced mobility and high metabolic risk. |
|
🟢 BCS 3 (5–7 in 9-point scale) = Ideal condition for health and reproduction. 🟡 BCS 2 or 4 = Borderline, requires monitoring (risk of under- or over-conditioning). 🔴 BCS 1 or 5 = Severe risk (malnutrition or obesity). | ||
Key Points for BCS Assessment (Where to Look and Feel)
The assessment of BCS involves the inspection and palpation of specific body locations:
- Backbone/Spine: The fat over the vertebrae is felt. It is checked whether they are sharp and prominent or smooth and not easily felt.
- Hips/Pins: The layer of fat covering the hip bones (Hook Bones and Pin Bones) is checked.
- Ribs: Feeling the ribs is most important. It involves seeing how much pressure is needed to feel the ribs.
- Tailhead: The amount of fat deposited around and over the tail is observed. In fat animals, the depression here fills up and a bulge appears.
- Shoulder and Neck: Primarily for assessing obesity.
- Hump: In Zebu cattle (e.g., Sahiwal, Gir, Tharparkar) and camels found in India and other hot climates, the hump is a primary site for the body’s energy reserves (fat). When the animal receives adequate nutrition, excess energy begins to be stored as fat, especially in the hump, around the tailhead, and near the shoulders. Therefore, the condition of the hump—by looking and touching—can provide an estimate of the status of the animal’s energy reserves.
Identify & Monitor At-Risk Animals
- Pay special attention to sheep/goats with twins/triplets, overweight/underweight, or those with problems in previous pregnancies.
- Blood Monitoring: In the last 4-6 weeks of pregnancy, check blood glucose (target > 40 mg/dL) and β-hydroxybutyrate (BHB; target < 0.8 mmol/L or 800 µmol/L) in at-risk animals. BHB > 1.0 mmol/L is a warning sign.
Stress Management and Early Intervention
- Stress Management: Avoid unnecessary stress (crushing, shearing, long-distance transport, sudden diet changes) in the late stage of pregnancy.
- Early Intervention: If any symptoms appear or BHB is elevated, immediately start Propylene Glycol (60 ml orally, twice a day) and an energy-dense diet. Consult a veterinarian.
Sample Collection for Accurate Diagnosis
- Blood:
- Serum: To measure glucose and β-hydroxybutyrate (BHB) levels (most important). In dry, cold tubes.
- EDTA/Heparin Plasma: To measure cortisol levels (less common). Centrifuge immediately and separate plasma.
- Fluoride Oxalate: Also for glucose (prevents glycolysis).
- Urine: For ketone bodies (ketonuria), fresh sample (Rothera’s test or dipstick).
Pregnancy toxemia is a preventable yet deadly disorder rooted in energy imbalance. Through vigilant nutrition, monitoring, and stress management, producers can safeguard flock health. Immediate treatment with energy substrates and parturition induction remains critical for affected animals.
THE RAJASTHAN EXPRESS