Downer Cow Syndrome (DCS): Definition, Causes, Symptoms, Diagnosis, and Treatment
Definition and Etiology of Downer Cow Syndrome
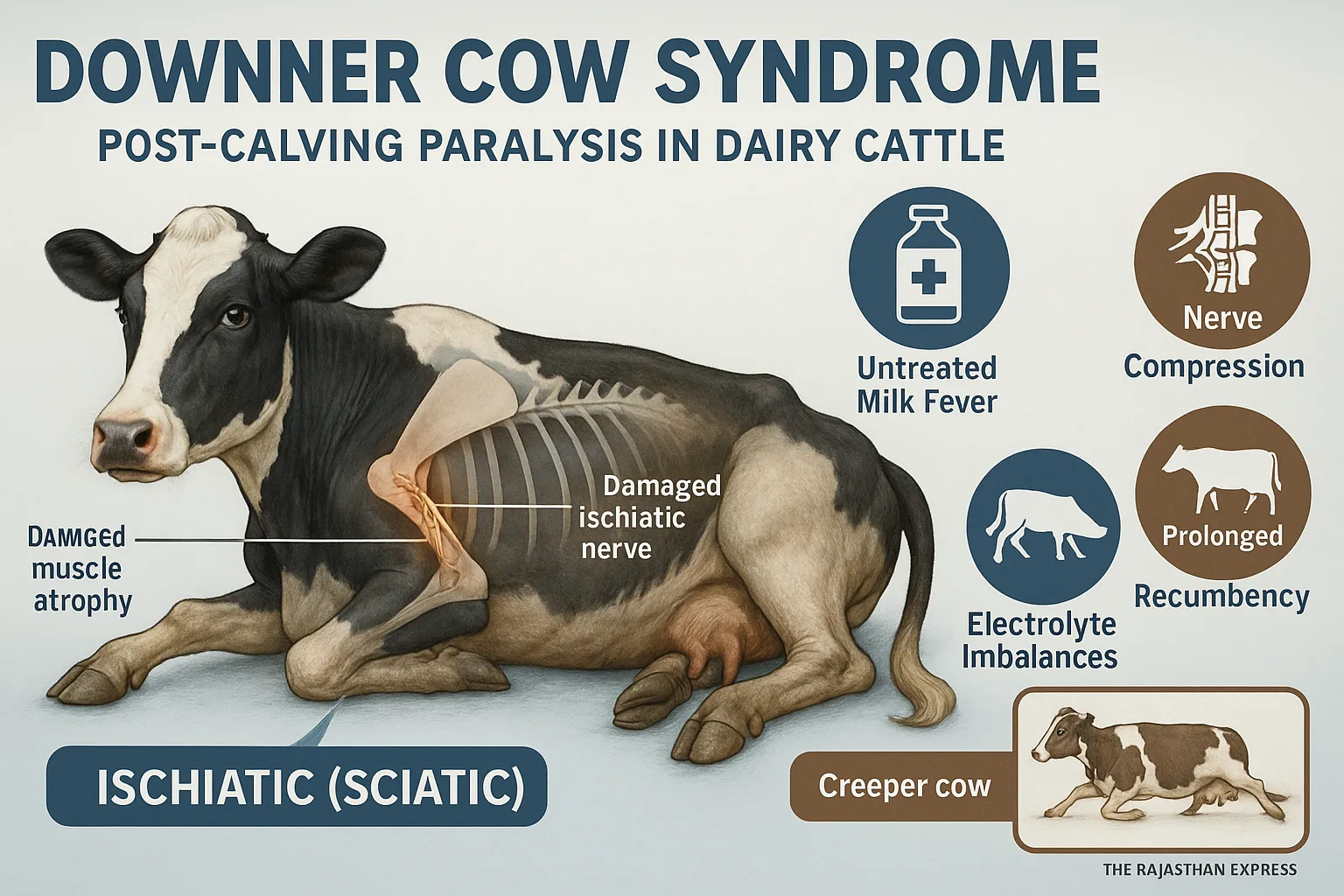
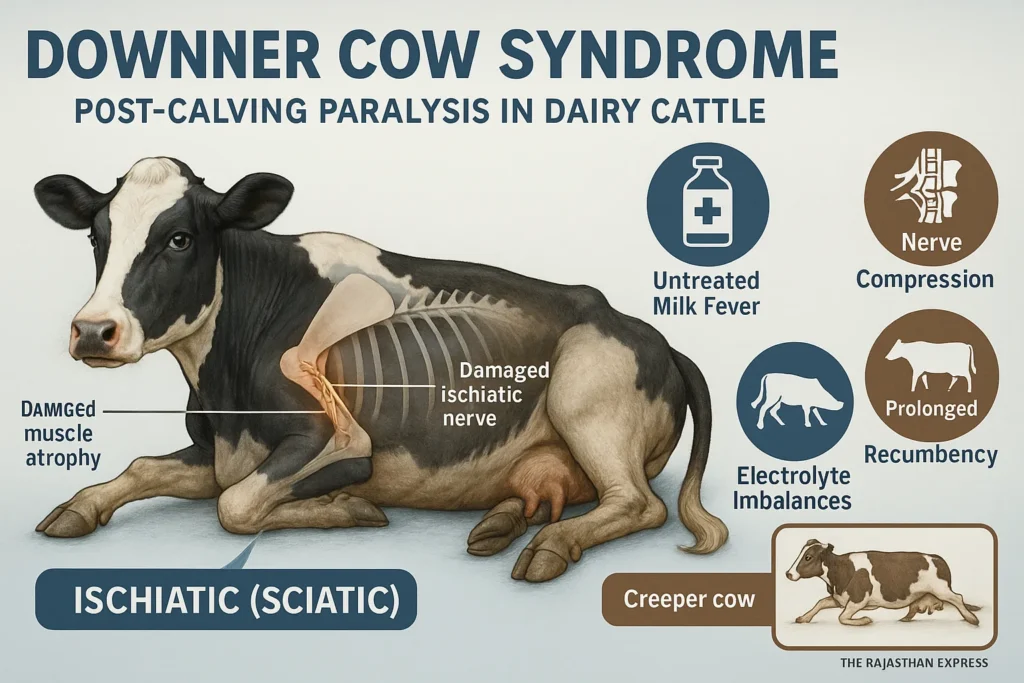
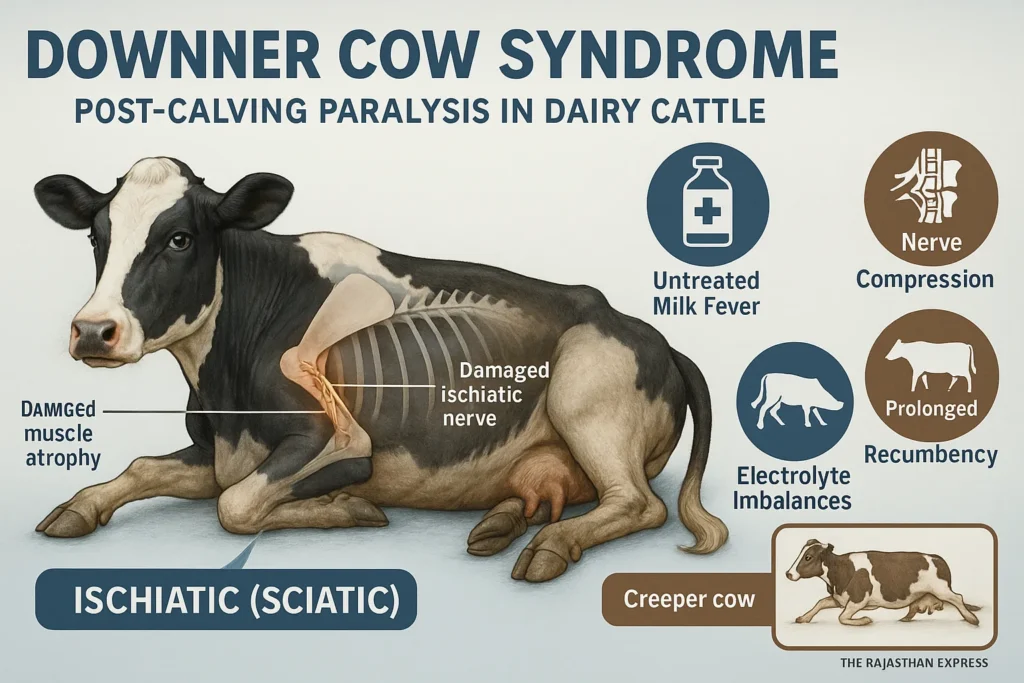
Downer Cow Syndrome (DCS) is a condition mainly observed in high milk-yielding dairy cows, typically within 2–3 days after calving. In this condition, the cow is unable to stand on its hind limbs.
This disease is most common in Holstein Friesian cows during their fifth lactation, when milk production peaks.
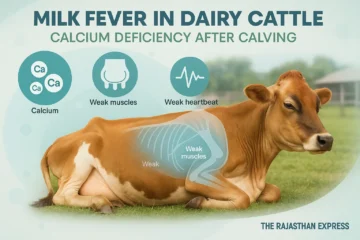
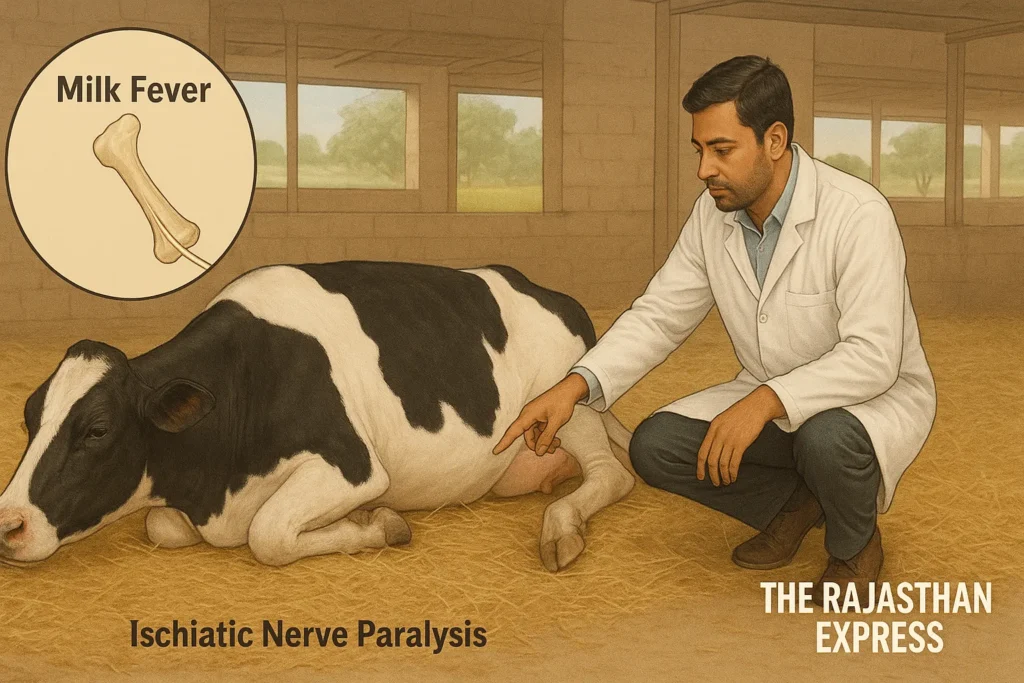
Downer Cow Syndrome is considered a severe complication of Milk Fever. If Milk Fever is not treated promptly and properly, the cow remains recumbent (lying down) for 2–3 days. This prolonged recumbency damages the Ischiatic Nerve, leading to muscle degeneration and paralysis of the hind limbs.
Downer Cow Syndrome (DCS)
| Also Known As | Postparturient Recumbency, Bovine Secondary Recumbency, Non-ambulatory Cow |
|---|---|
| Definition | Inability of a dairy cow (typically within 2–3 days postpartum) to rise and stand, despite being alert and otherwise physiologically normal. Often a sequel to metabolic disorders or trauma. |
| Etiology & Pathophysiology | Secondary to unresolved Milk Fever and prolonged recumbency causing muscle ischemia and sciatic (ischiatic) nerve damage. Contributing factors include hypocalcemia, hypomagnesemia, hypophosphatemia, hypokalemia, and sometimes pelvic trauma or dystocia. |
| Risk Factors |
|
| Clinical Presentations |
|
| Diagnosis |
|
| Differential Diagnoses |
|
| Treatment & Nursing Care |
|
| Prevention & Management |
|
| Prognosis | Depends on duration of recumbency and response to treatment. Delay beyond 24 hours often results in decreased survival; after 7 days, survival drops sharply due to organ failure and pressure damage. |
| Regulatory & Welfare Considerations | In the U.S., non-ambulatory (“downer”) cows may not be sold for human consumption due to animal welfare and food safety regulations (USDA policy, BSE concerns) |
| Sources: Merck Veterinary Manual;University Extension Services (UI, VT); Iowa State Organic Livestock Guidance; The Rajasthan Express | |
The Ischiatic Nerve is the largest nerve in the body, and when damaged, the hind limbs lose sensitivity. If only calcium (Ca) is administered during Milk Fever treatment but the animal remains recumbent for too long, it can develop into Downer Cow Syndrome.
This condition is not caused by calcium deficiency alone. Deficiencies of magnesium (Mg), phosphorus (P), and potassium (K) are also involved. Therefore, treatment must include a combined electrolyte balance (Na, K, Mg, Ca) along with Vitamin E supplementation.
Excessive and repeated calcium administration during Milk Fever may elevate blood calcium to dangerous levels, causing myocarditis (inflammation of heart muscles) due to calcium overdose.
In Downer Cow Syndrome in cattle, the animal otherwise remains alert—eating, drinking, and excreting normally—but cannot rise on its hind limbs. Such cows may attempt to crawl with their forelimbs, a condition termed “Creeper Cow.”
Sometimes, trauma to the pelvic muscles or nerves before or during calving can also lead to this syndrome.
Metabolic Disease in Animals: Definition, Types, and Key Characteristics
Definition:
Metabolic Diseases are those diseases which occur due to deficiency, imbalance of nutrients, or disturbance of metabolism in the body. These diseases are especially related to milk production, pregnancy, and the energy requirements of the body.
Read More About : Metabolic Disease
Main Features of Metabolic Disease in Dairy Cattle
- These diseases are Non-Contagious — do not spread from one animal to another.
- In most cases, these diseases are related to the production system, hence they are also called Production Diseases.
- Especially pregnant and milk-producing animals (like cow and buffalo) are more susceptible to these diseases.
- The possibility of metabolic diseases increases with increasing milk production.
- In native cows (Zebu cattle), the highest possibility of metabolic disease is found in the third calving.
- In exotic cows (Exotic Cattle), this possibility is highest in the fifth calving.
- In buffaloes, the possibility of metabolic diseases is mostly in the fourth calving.
- The order of possibility of metabolic diseases is as follows:
Exotic Cow > Native Cow > Buffalo - The possibility of Downer Cow Syndrome, Ketosis, Postpartum Haemoglobinuria, and Mastitis disease is higher in exotic cows, especially in the Holstein-Friesian breed.
- These same diseases are found mostly in the Sahiwal breed in native cows.
- The possibility of Milk Fever is highest in Jersey cows.
We have also explained these diseases in detail.
Explore the key metabolic diseases in cattle with quick links to each section:
- Milk Fever – Calcium deficiency immediately after calving
- Downer Cow Syndrome – Complications from prolonged lying after milk fever
- Ketosis In Cattle – Energy deficiency and ketone accumulation
- Postparturient Haemoglobinuria – Red blood cell destruction due to phosphorus deficiency
- Grass Tetany – Muscle cramps from magnesium deficiency
- Pregnancy Toxemia – Energy deficiency in late pregnancy
Other Names for Downer Cow Syndrome
Downer Cow Syndrome is also known as Postparturient Recumbency, as it occurs after calving and cows remain lying on one side.
Predisposing Factors of Downer Cow Syndrome
- Delayed (stage three) treatment of Milk Fever
- Prolonged lateral recumbency during Milk Fever
- Trauma to the sciatic nerve and pelvic muscles
- Electrolyte imbalance (Na, K, Mg, Ca)
- Slippery floors increasing risk of falls
Clinical Signs of Downer Cow Syndrome
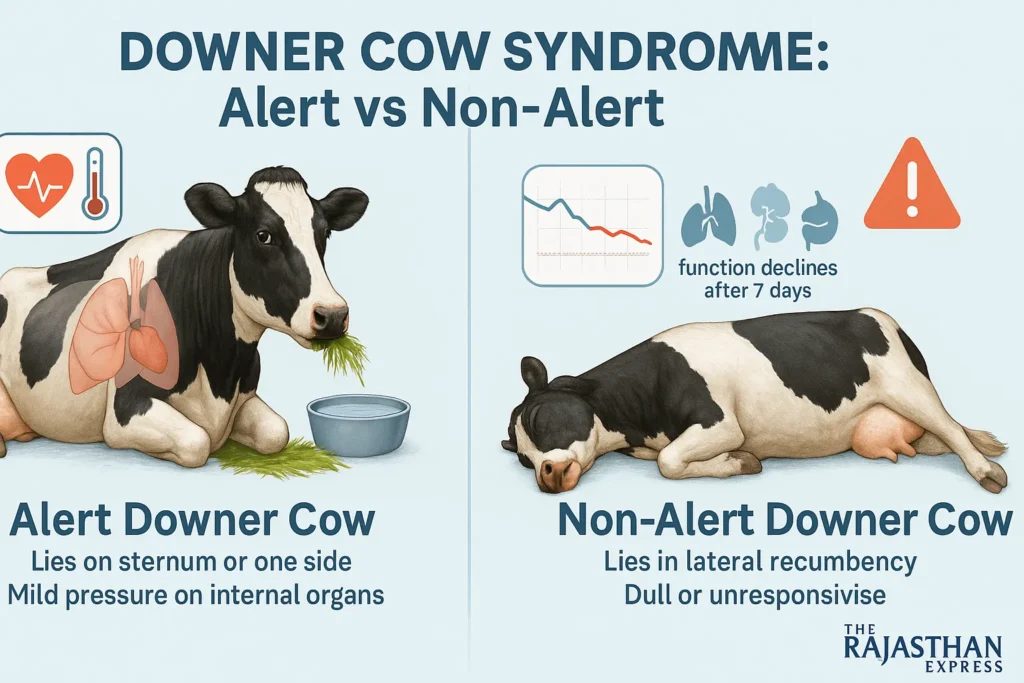
1. Alert Downer Cow
- The animal remains in sternal or lateral recumbency, causing prolonged pressure on internal organs (heart, liver, lungs).
- Eats and drinks normally.
- Pulse and heart rate are normal in the early stage, but increase as the disease progresses.
- Body temperature remains normal (~101.5°F) initially but becomes subnormal in the terminal stage.
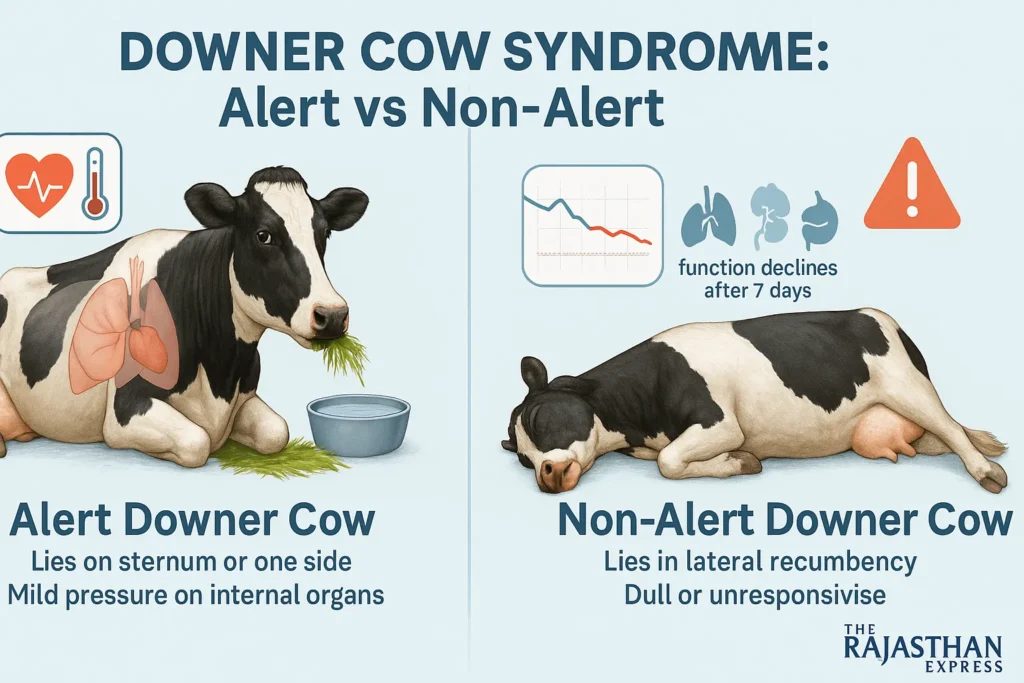
2. Creeper Cow Condition
An alert downer cow that attempts to crawl using forelimbs to rise is termed a Creeper Cow.
3. Non-Creeper Cow
The cow remains alert but makes no attempt to rise. This suggests severe nerve damage and loss of sensation.
4. Non-Alert Downer Cow
- The animal stops eating and drinking.
- Gradually slips into a coma-like state.
- Lies on one side (lateral recumbency), hence also called Postparturient Recumbency.
If the cow remains down for 7 days or more, the functioning of heart, kidneys, and lungs is severely compromised, drastically reducing survival chances.
Diagnosis of Downer Cow Syndrome
- Recent history of calving, dystocia (difficult birth), and prolonged recumbency.
- Elevated muscle enzymes CPK (normal: 40–280 IU/L) and AST.
- Low levels of calcium, phosphorus, and magnesium in serum.
- Untreated or improperly treated Milk Fever.
- Presence of mild to moderate proteinuria and ketonuria.
- Postmortem reveals hemorrhage and degeneration of thigh muscles.
- If the cow cannot rise despite Milk Fever treatment, it is diagnosed as Downer Cow Syndrome in cattle.
Differential Diagnosis of DCS in Cattle
- Coliform Mastitis
- High fever, discolored milk, swollen udder
- Bone Fractures
- Hip bone or femur fractures confirmed by radiography
Downer Cow Syndrome Treatment
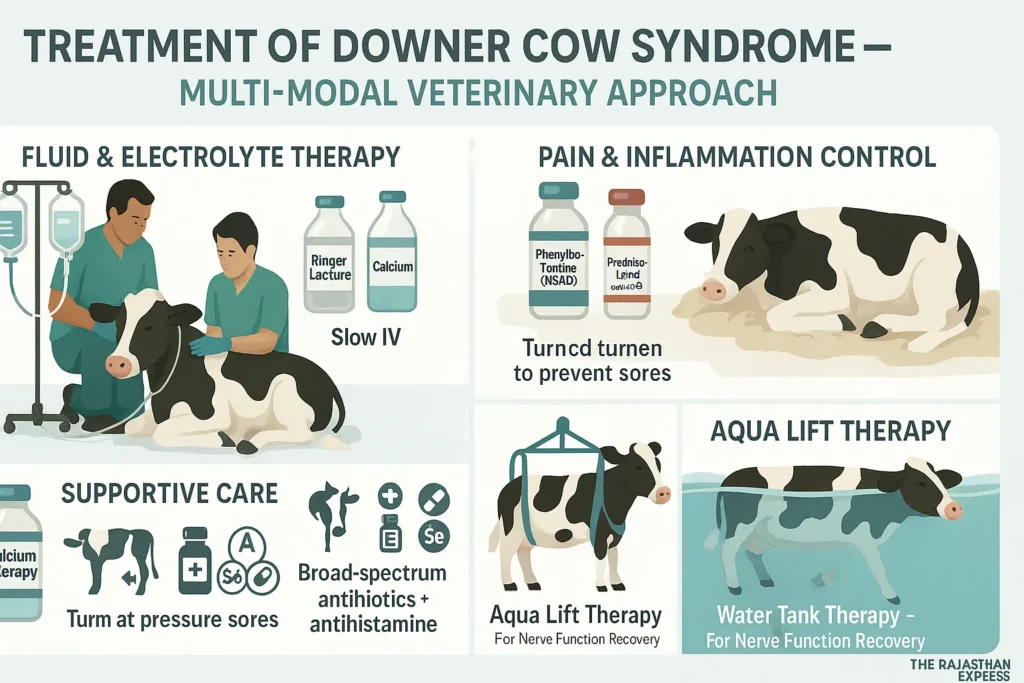
1. Fluid and Electrolyte Therapy
- IV infusion of Isotonic Ringer Lactate, Calcium, and Magnesium
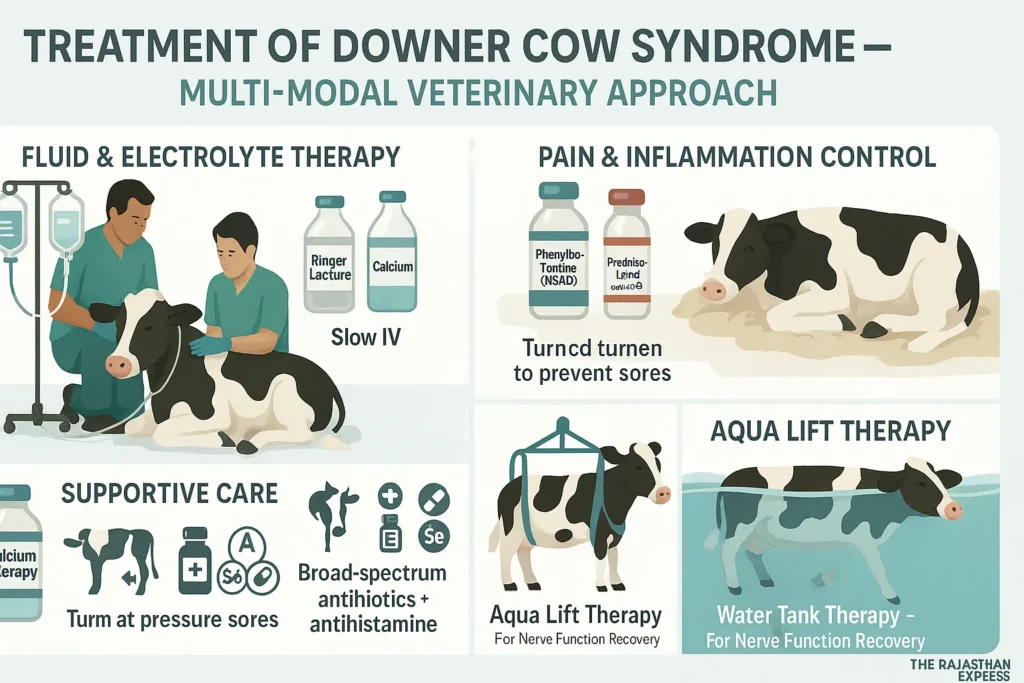
2. Pain Relief and Anti-Inflammatory Drugs
- NSAIDs (e.g., Phenylbutazone)
- Steroids (Prednisolone)
3. Supportive Care
- Provide comfortable bedding
- Change sides multiple times daily to prevent pressure sores
- Use slings or lifting machines to assist standing
- Vitamin E, Selenium, and Antihistamines
4. Aqua Lift Therapy
The cow is placed in a water tank to float, reducing body weight load and helping restore nerve function.

Prevention and Control of Downer Cow Syndrome
- Prognosis depends on the underlying cause of recumbency.
- Early and proper treatment of Milk Fever, along with providing soft bedding, can prevent Downer Cow Syndrome in buffalo and cows.

Difference Between Milk fever and Downer Cow Syndrome
| Difference Between Milk fever and Downer Cow Syndrome : The Rajasthan Express | ||
| Parameter | Milk Fever (Hypocalcemia) | Downer Cow Syndrome (DCS) |
|---|---|---|
| Definition | Acute calcium deficiency (<5.5 mg/dL) due to excessive calcium loss in colostrum. | Secondary complication from prolonged recumbency (>24 hours), often following untreated milk fever, causing nerve/muscle damage. |
| Primary Cause | Sudden calcium demand for colostrum production exceeding mobilization capacity. | Untreated milk fever, trauma during calving, or electrolyte imbalances (Ca, P, Mg, K) leading to sciatic nerve damage. |
| Onset | Within 72 hours post-calving (occasionally 2–3 days pre-calving). | Develops 2–3 days post-calving after prolonged recumbency (>24 hours). |
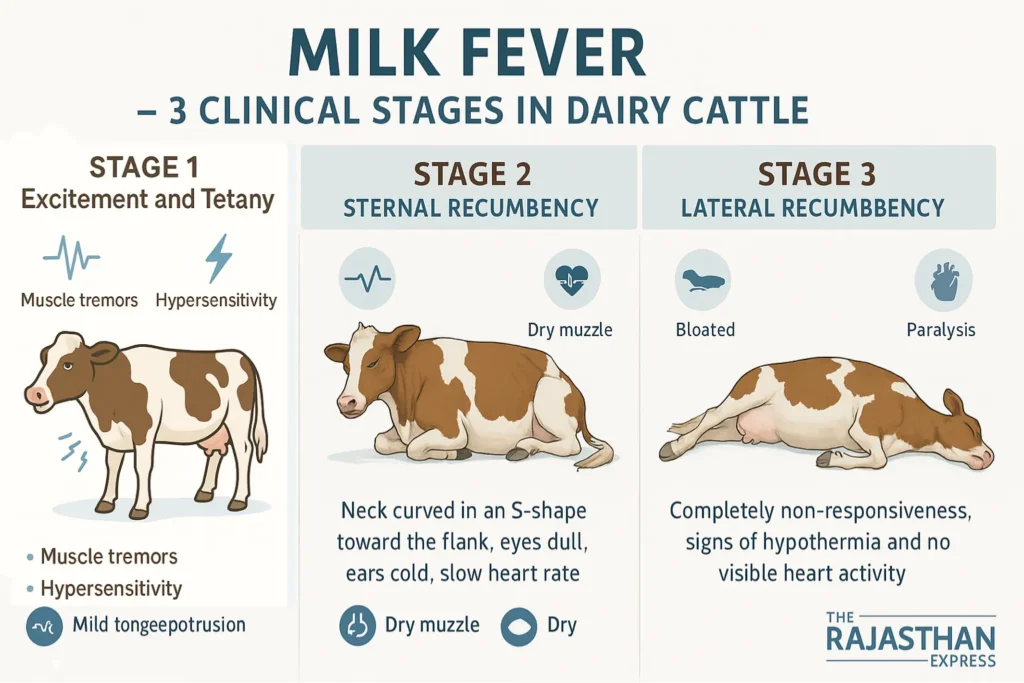
| Key Clinical Signs |
Stage 1: Muscle tremors, restlessness. Stage 2: Sternal recumbency, “S-bend neck,” hypothermia. Stage 3: Lateral recumbency, coma. |
Alert DCS: Eats/drinks normally but cannot stand. Creeper Cow: Crawls using forelimbs. Non-alert DCS: Coma, organ failure. |
| Diagnosis |
– Blood Ca²⁺ <5 mg/dL. – Sulkowitch urine test (low calcium). – Clinical signs (e.g., “S-bend neck”). |
– Elevated CPK (>1000 IU/L) and AST (>500 IU/L). – History of dystocia or untreated milk fever. – Myoglobinuria (brown urine). |
| Treatment | IV 23% calcium borogluconate (250 mL IV + 200 mL SC). Supportive: Magnesium sulfate SC to prevent tetany. | Multimodal: – Electrolyte fluids (Ca, Mg, P). – NSAIDs (phenylbutazone). – Nursing care (slings, side rotations). – Aqua lift therapy. |
| Breeds at Risk | Jersey > Holstein > Exotic breeds (peak at 5th lactation). | Holstein-Friesian (5th lactation) > Buffaloes. |
| Prevention | DCAD diets pre-calving (anionic salts). Oral calcium boluses at calving. Vitamin D₃ supplementation. | Prompt milk fever treatment (within 4–6 hours). Soft bedding to avoid pressure injuries. Avoid over-conditioning pre-calving. |
| Prognosis | Excellent if treated early (90% recovery). | Guarded (30–50% recovery if recumbent >7 days). |
| Economic Impact | $334/case (milk loss, treatment costs). | >$1000/case (extended care, culling). |
| Key Pathophysiological Differences | ||
| Mechanism of Recumbency | Flaccid paralysis due to hypocalcemia impairing neuromuscular function. | Ischemic muscle/nerve damage (sciatic compression) from prolonged recumbency. |
| Electrolyte Involvement | Primarily calcium deficiency (Ca²⁺ <1.6 mmol/L). | Multifactorial: Ca, P, Mg, K deficiencies + muscle enzyme leaks (CPK/AST). |
| Response to Treatment | Rapid improvement post-calcium infusion (stands within 1–2 hours). | Requires days of rehabilitation; success depends on early intervention. |
| Difference Between Milk fever and Downer Cow Syndrome : The Rajasthan Express | ||
Read More About : Milk Fever in Cattle
🔥 Q: If calcium fixes Milk Fever, why is it causing Downer Cow deaths?
A: Emerging research reveals a dangerous paradox: Standard calcium (Ca) therapy for Milk Fever (hypocalcemia) can trigger Downer Cow Syndrome (DCS) through cardiotoxicity, nerve damage, and mineral imbalances. Here’s why:
💔 1. Calcium Overcorrection → Cardiac Stress & Myocarditis
- Mechanism: Rapid IV calcium floods the bloodstream, spiking levels to 5–10× normal. This overwhelms cardiac cells, causing:
- “Heart blockade”: Transient high Ca²⁺ disrupts electrical conduction, risking arrhythmia or arrest .
- Inflammation: Ca²⁺ overload triggers immune cells to release cytokines, damaging heart muscle (myocarditis) .
- Evidence: Autopsies of DCS cows show myocardial necrosis linked to repeated Ca injections .
⚠️ Controversy: 68% of DCS cases trace to improper Milk Fever protocols—often aggressive IV calcium without monitoring .
🦵 2. Prolonged Recumbency → Ischiatic Nerve Paralysis
- Sequence of failure:
- Delayed/inadequate Milk Fever treatment → cow remains down >6 hours.
- Body weight crushes the ischiatic nerve (body’s largest nerve) against hard surfaces.
- Nerve ischemia → demyelination → permanent hindlimb paralysis .
- Calcium’s role: Treating only hypocalcemia ignores co-factors like phosphorus (P) deficiency, which impairs nerve repair. Cows with blood P <0.9 mmol/L are 12× more likely to develop DCS .
| Blood Mineral Thresholds Linked to DCS Risk | |||
| Mineral | Safe Level | Danger Zone | DCS Risk Multiplier |
|---|---|---|---|
| Calcium | >1.7 mmol/L | <1.4 mmol/L | 14× |
| Phosphorus | >0.9 mmol/L | <0.5 mmol/L | 12× |
| Magnesium | >0.85 mmol/L | <0.75 mmol/L | 3× |
| Blood Mineral Thresholds Linked to DCS Risk : The Rajasthan Express | |||
Source: The Bullvine – Trouble-shooting Milk Fever and Downer Cow Problems & PMCID: PMC1852599
⚖️ 3. Mineral Imbalances: Ignoring Phosphorus & Potassium
- Phosphorus (P) depletion:
- 80% of Milk Fever cows have hypophosphatemia. Low P cripples ATP production, preventing muscle contraction needed to stand .
- Ca injections worsen this: Calcium binds phosphate, forming insoluble complexes that reduce bioavailable P .
- Potassium (K) disruption:
- Hypocalcemia alters K⁺/Na⁺ pumps. Sudden Ca correction causes extracellular K⁺ shifts → muscle weakness .
- Solution: Combined Ca-Mg-P solutions (e.g., Cal-Dextro) reduce DCS by 40% vs. calcium-only products .
🧬 4. The Inflammation Paradox: Calcium as Immune Moderator
Groundbreaking research (Calci-Inflammatory Network theory) suggests hypocalcemia may be the cow’s adaptive response to calving inflammation 69:
- Low blood Ca²⁺ dampens immune cell activation, preventing destructive inflammation (e.g., mastitis, metritis).
- Artificially spiking Ca with IV infusions disrupts this balance → unleashes unchecked inflammation → tissue damage → DCS.
💡 Game-changer: Precision calcium dosing (e.g., oral boluses + IV only for critical cases) aligns with the cow’s immune state, cutting DCS by 60% .
🌟 Prevention Over Cure: Avoiding the Calcium Trap
- DCAD diets: Feed negative DCAD rations pre-calving (-50 to -150 mEq/kg) to activate Ca mobilization before birth .
- Subcutaneous/oral Ca: Safer than IV; avoids spikes. Use 75g calcium boluses at calving .
- Phosphorus boosters: Add monosodium phosphate to fresh-cow rations .
- Blood testing: Check Ca, P, Mg before treating. If P <1.3 mmol/L, supplement immediately .
| DCS Prevention Protocol | ||
| Timeline | Action | DCS Reduction |
|---|---|---|
| 3 weeks pre-calving | Negative DCAD diet | 70% |
| At calving | 2× oral calcium boluses (12h apart) | 50% |
| 1 hour post-calving | Blood test: Ca, P, Mg | 85% |
| Recumbency >2h | Sling support + Aqua Lift therapy | — |
| DCS Prevention Protocol : The Rajasthan Express | ||
Source : PMCID: PMC11687054 PMID: 39736605
💎 The Bottom Line
Calcium isn’t a “cure-all” for Milk Fever—it’s a double-edged sword. Downer Cow Syndrome often stems from:
- Overzealous IV calcium → heart stress,
- Ignoring phosphorus → nerve failure,
- Disrupting the body’s inflammatory control.
Revolutionary approach: Treat inflammation, not just calcium. The future lies in precision mineral therapy guided by on-farm blood testing .
🌐 Human health link: This paradigm applies to ICU patients with sepsis or COVID-19, where forced calcium correction worsens outcomes. Cows are teaching us to rethink inflammation! .
“Milk Fever treatment mistakes causing Downer Cow Syndrome? Discover why calcium overdose destroys nerves, the 7-day survival window, and how Aqua Lift therapy saves 40% more cows. Prevention checklist included.”
THE RAJASTHAN EXPRESS
Frequently Asked Questions About Downer Cow Syndrome (DCS)
What specific clinical signs differentiate primary vs. secondary downer cow syndrome beyond 24 hours?
- Primary DCS (First 24h):
- Caused by hypocalcemia, dystocia trauma, or toxemia
- Cows remain alert with normal TPR
- Often attempt to crawl (“creeper” behavior)
- Maintain appetite and hydration
- Secondary DCS (>24h):
- Caused by pressure-induced muscle/nerve damage
- Transition from “creeper” to non-creeper
- Diminished pain response in hind limbs
- Rising CK/AST levels (muscle injury)
- Brown urine (myoglobinuria)
- Late signs: subnormal temperature, elevated pulse
Can downer cow syndrome occur in buffalo, and how does management differ from cattle?
- Occurrence: Yes – buffalo experience DCS from similar periparturient causes
- Management similarities:
- Same electrolyte correction protocols (Ca, P, K, Mg)
- Identical nursing requirements: deep bedding, frequent rolling
- Equivalent lifting precautions
- Key difference: No special adaptations needed – follow cattle protocols per India’s DAHD guidelines
What is the evidence for phosphorus/potassium supplementation in non-responsive downer cows?
- Hypophosphatemia link: Cows with serum P <0.9 mmol/L are 12× more likely to become downers
- 2023 Clinical Protocol:
- Oral di-potassium phosphate bolus after calcium treatment
- Effective dosing: P (4.5–7.5g/day), K (60–120g/day)
- Critical monitoring: Track CK levels and urine pH
- USDA-validated: Electrolyte balancing is essential when calcium alone fails
Why is hip clamp use controversial, and what are safer alternatives?
- Risks:
- Bruising/crushing of soft tissues
- Worsened sciatic nerve damage
- Rib fractures with improper use
- Safer alternatives:
- Canvas slings with sternum support: Distributes weight naturally
- Float tank therapy: 47% recovery rate in clinical settings
- Frequent rolling: Prevents pressure injuries
- If used: Limit to <5 minutes, 2-3×/day with immediate stop at discomfort signs
What are optimal bedding materials for downer cows?
- Deep sand (gold standard):
- Lowest pressure sore risk
- Best bacterial hygiene
- Higher manure handling costs
- Deep straw (practical alternative):
- Moderate pressure relief
- Lower cost than sand
- Requires frequent refreshing
- Manure pack (avoid if possible):
- High infection risk when wet
- Increased dermatitis cases
How often should you roll a downer cow?
- Ideal interval: Every 3-4 hours
- Critical factors:
- Shorter intervals (3h) for heavy cows or poor bedding
- Longer intervals (4-6h) acceptable on deep sand
- Purpose: Prevents pressure-induced muscle ischemia and nerve compression
When is euthanasia ethically required for downer cows?
- Poor prognosis indicators:
- >7 days recumbency with no improvement
- Non-alert mental state
- Infected decubital ulcers
- Organ failure signs (renal/pulmonary)
- Recovery probability:
- Days 1-2: 75% survival
- Day 7+: <10% survival
- Ethical threshold: No meaningful improvement by day 7 warrants euthanasia
Does DCS increase HPAI (avian influenza) risk in dairy cows?
- No evidence linking recumbency to increased HPAI transmission
- Primary risks:
- Contaminated milking equipment
- Animal movement between farms
- Wild bird exposure
- Biosecurity focus should prioritize milking hygiene over recumbency status
Will 2025 genetic changes increase DCS rates?
- Genetic update (2025): CDCB base change only rescales PTAs – doesn’t alter biological risk
- DCS prevention requires:
- Selection for robust Hypocalcemia PTAs
- Prioritizing transition cow management
- Monitoring electrolyte balance pre-calving
- High-merit herds must balance production traits with health indices