Diabetic Ketoacidosis in Cats: Symptoms, Treatment, and Survival Guide
What is Diabetic Ketoacidosis (DKA) in Cats?
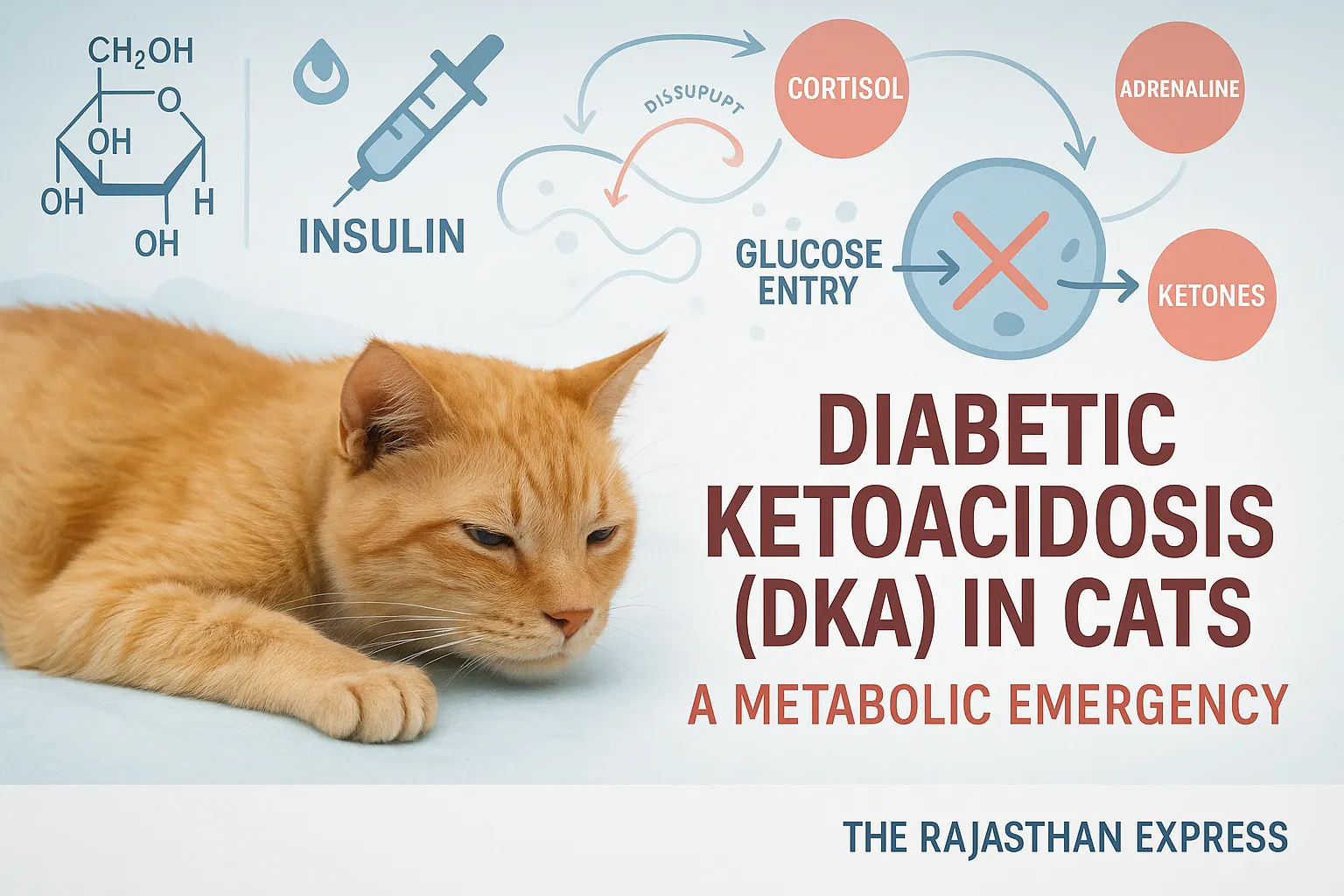
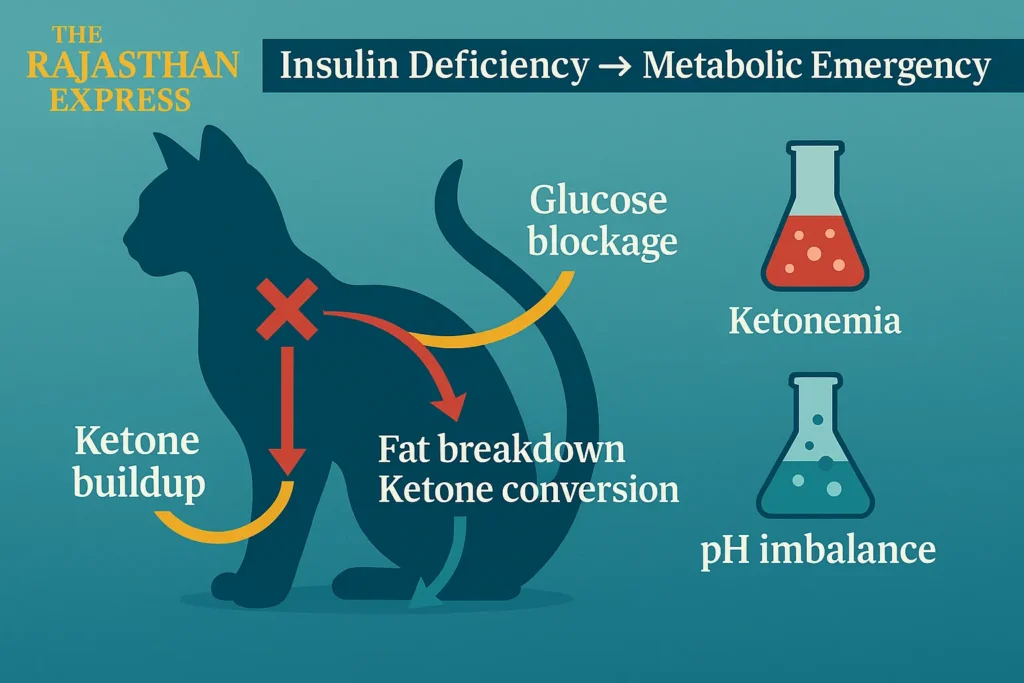
Diabetic ketoacidosis (DKA) is a serious metabolic emergency. This condition arises when normal metabolism of glucose does not occur due to extreme deficiency of insulin or insulin resistance in the body.
If diabetes in cats is not treated timely and appropriately, glucose cannot reach cells due to insulin deficiency or insulin resistance. When an existing illness—such as infection, inflammation, or stress—increases the body’s metabolic rate, energy demand also rises. To meet this increased demand, the body produces stress hormones (e.g., cortisol, adrenaline), which further reduce insulin’s effectiveness.
In this situation:
- Cells cannot utilize glucose for energy.
- The body starts breaking down fat to produce ketone bodies.
- This increases ketone levels in blood and urine, termed ketonemia and ketonuria respectively.
Diabetic Ketoacidosis (DKA) in Cats
| Medical Term | Feline Diabetic Ketoacidosis (DKA) |
|---|---|
| Condition Type | Acute Metabolic Emergency |
| Species Affected | Domestic Cats (Felis catus) |
| Cause | Severe insulin deficiency or insulin resistance |
| Primary Pathology |
|
| Hormonal Imbalance |
|
| Clinical Symptoms |
|
| Diagnostic Criteria |
|
| Gold Standard Tests |
|
| Essential Bloodwork |
|
| ATP Production Impact |
|
| Emergency Treatment |
|
| Monitoring Frequency |
|
| Glucometer for Cats |
|
| Prognosis |
|
| DKA vs. HHS (Comparison) |
|
| Common Triggers |
|
| Storage Molecules |
|
| Prevention Tips |
|
| Diabetic Ketoacidosis in Cats: The Rajasthan Express | |
Cat Diabetic Ketoacidosis Symptoms and Key Causes
Diabetic ketoacidosis (DKA) does not result from a single cause but develops due to a combination of factors. Key contributors include:
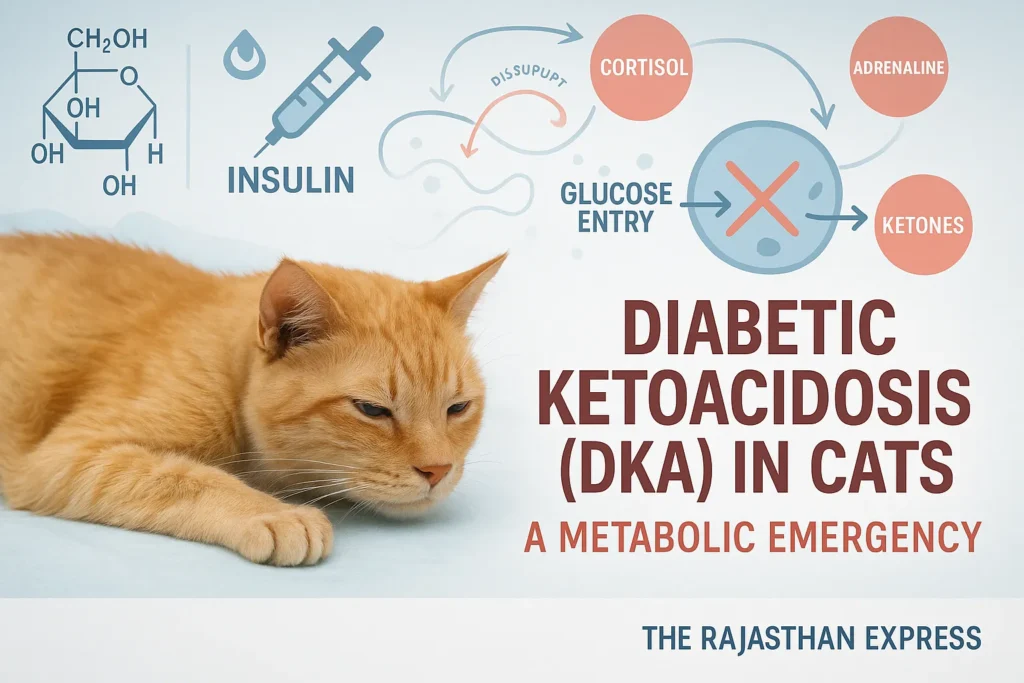
1. Hyperglycemia (High Blood Glucose)
- When insulin deficiency or insulin resistance occurs, glucose cannot enter cells. This abnormally elevates blood glucose levels.
2. Ketone Body Accumulation
Fat breakdown for energy produces three types of ketone bodies:
- Beta-hydroxybutyrate (β-Hydroxybutyrate)
- Acetoacetate
- Acetone
Excessive levels disrupt the body’s acid-base balance, causing metabolic acidosis.
3. Metabolic Acidosis
- The body’s pH decreases.
- Blood becomes more acidic.
- This affects nervous system functionality and organ performance.
4. Dehydration
- Hyperglycemia increases urine output (osmotic diuresis), leading to fluid and electrolyte loss.
5. Electrolyte Imbalance
- Excessive potassium (K⁺) and phosphate (PO₄³⁻) loss through urine.
- Levels drop rapidly during insulin therapy, severely impacting the heart, muscles, and nerves.
Summary: DKA is a multi-causal disease involving high blood sugar, ketone buildup, acidosis, dehydration, and electrolyte imbalance. Each factor exacerbates the others, worsening the condition.
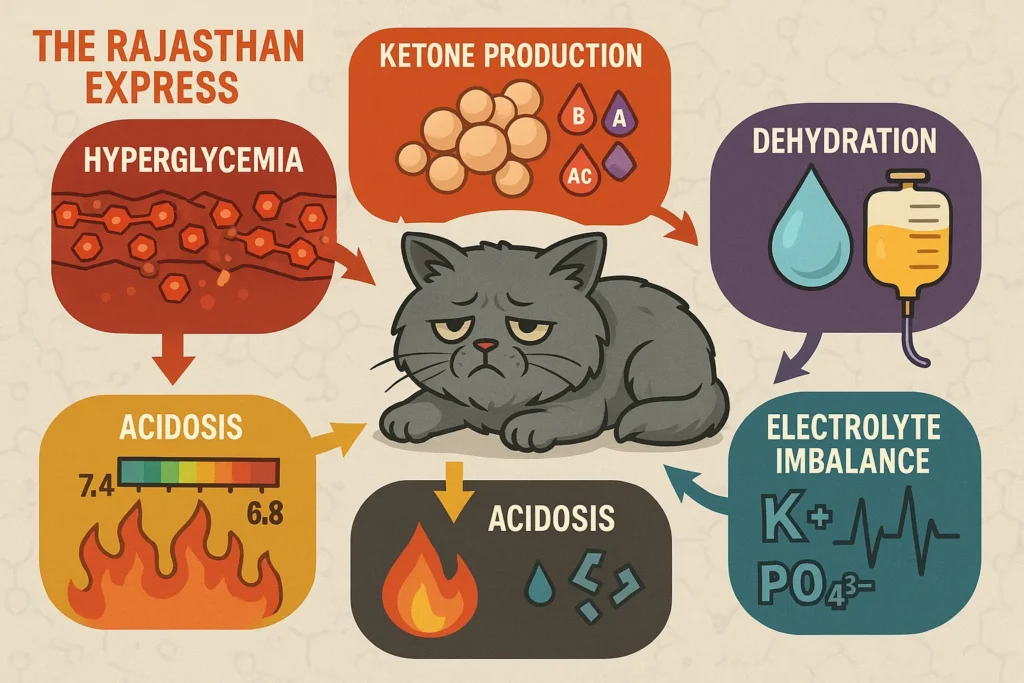
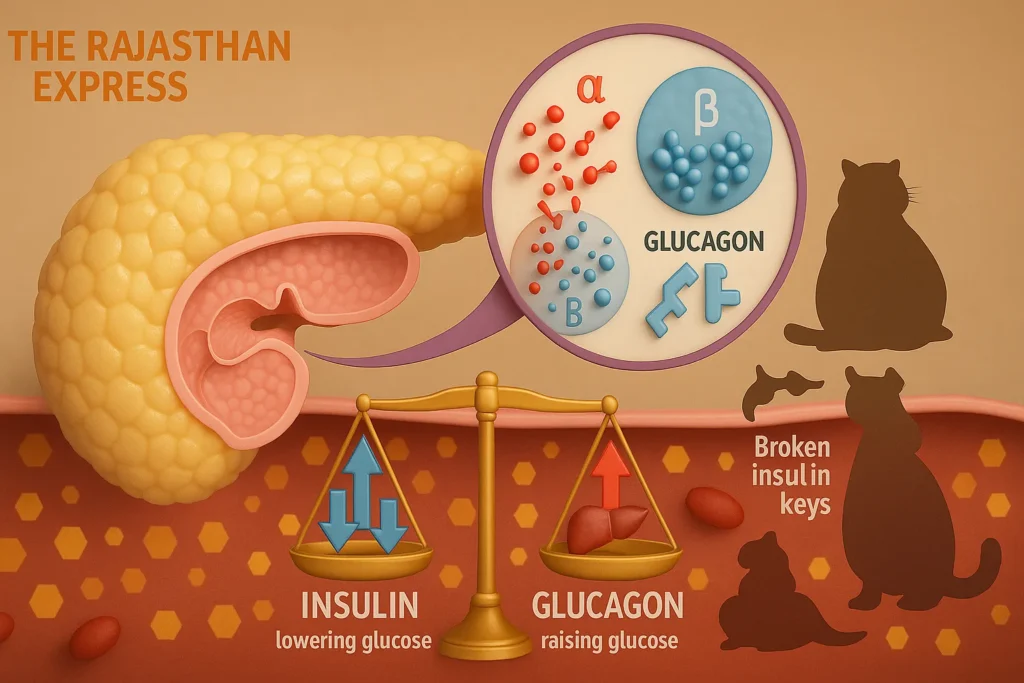
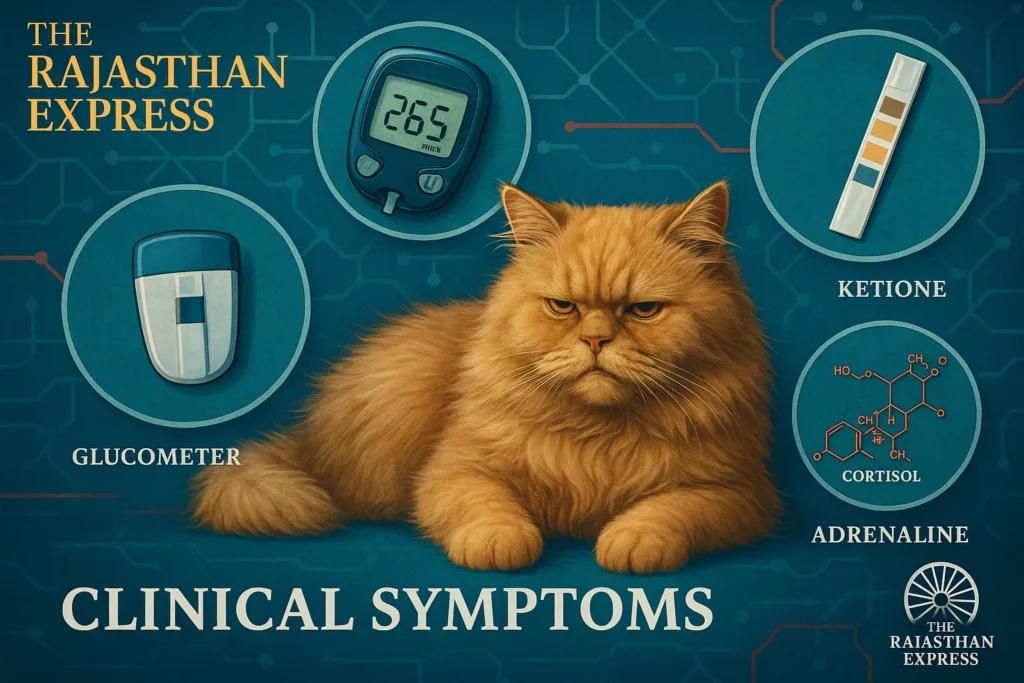
The Role of Hormones in DKA
Insulin and glucagon—both secreted by the endocrine pancreas (Islets of Langerhans)—perform opposing functions:
- Glucagon: Released by alpha (α) cells, increases blood glucose.
- Insulin: Released by beta (β) cells, decreases blood glucose.
If insulin is deficient or ineffective (e.g., due to obesity), blood glucose rises, triggering diabetes symptoms.
Diabetic Ketoacidosis in Cats Treatment Approach
Effective DKA treatment requires addressing all underlying factors—not just one. Veterinarians must first identify root causes (e.g., infection, pancreatitis) that trigger or worsen DKA before initiating therapy.
DKA Cat Bloodwork and Core Treatment Components
1. Intravenous Fluid Therapy (IV Fluids)
- Replenishes dehydration and improves blood circulation.
- Crystalloids (e.g., 0.9% NaCl) are commonly used.
2. Insulin Therapy
- Short-acting insulin (e.g., Regular Insulin) controls blood glucose.
- Initial IV/IM administration; switched to subcutaneous (SC) once glucose stabilizes.
3. Electrolyte Supplementation
- Potassium (K⁺) and phosphorus (PO₄³⁻) levels must be maintained.
- Sodium, magnesium, and chloride levels should also be monitored.
4. Treating Underlying Causes
- Essential if triggered by infection, pancreatitis, cancer, or systemic diseases.
5. Continuous Monitoring and DKA Cat Bloodwork
Critical parameters to track during treatment:
- Blood glucose: Every 1–2 hours.
- Ketone levels: Via urine/blood tests.
- Acid-base balance (pH): Through blood gas analysis.
- Electrolytes: Especially potassium and phosphorus.
6. Diabetic Ketoacidosis in Cats Survival Rate and Prognosis
Successful DKA treatment extends beyond insulin administration. It is a holistic process involving:
- Fluid balance restoration
- Electrolyte stability
- Identification/treatment of root causes
- Rigorous monitoring
Conclusion: Timely, coordinated treatment reduces DKA severity in cats and can save lives.
Pathophysiology of Diabetic Ketoacidosis in Cats
Glucose is the primary source of carbohydrates. It is a monosaccharide sugar and an example of a hexose sugar. In non-ruminant animals, glucose is the final product of carbohydrate digestion.
Carbohydrates are stored as glycogen in animals. This is the body’s main energy source, enabling mitochondria within cells to produce energy molecules called Adenosine Triphosphate (ATP).
ATP is obtained through aerobic and anaerobic oxidation of glucose.
- One glucose molecule produces approximately 32 ATP under aerobic conditions.
- Only 2 ATP are produced under anaerobic conditions.
ATP Production Process (Aerobic Conditions):
- Glycolysis (in cytoplasm):
Glucose → 2 Pyruvic Acid + 2 ATP + 2 NADH - Link Reaction (in mitochondrial matrix):
2 Pyruvic Acid → 2 Acetyl-CoA + 2 NADH - Krebs Cycle:
2 Acetyl-CoA → CO₂ + H₂O + 2 ATP + 6 NADH + 2 FADH₂ - Electron Transport System (ETS):
- 1 NADH = 2.5 ATP
- 1 FADH₂ = 1.5 ATP
Total ATP Calculation: 32 ATP
In humans and pets, carbohydrates are stored as glycogen. During fasting, glycogen converts to glucose via glycogenolysis (primarily in the liver). Similarly, excess body fat is stored as Triacylglycerol (TAG). During starvation, TAG breaks down into fatty acids via lipolysis. These fatty acids convert to Acetyl-CoA:
- Some enter the Krebs Cycle to produce energy.
- Others form ketone bodies (acetoacetate, beta-hydroxybutyrate, acetone).
Excess Ketone Bodies Cause:
- Ketonemia (in blood)
- Ketonuria (in urine)
Collectively termed Ketosis.
Insulin-Glucose Relationship
To produce ATP, cells require insulin (except brain cells) to transport glucose from blood. Inside cells, glucose either:
- Generates ATP, or
- Stores as glycogen (liver/muscles) or fat (triglycerides).
- Insulin also transports electrolytes (e.g., potassium) into cells and inhibits fat oxidation.
Diabetes Mellitus (DM) occurs due to:
- Insulin deficiency
- Impaired insulin receptor function
- Reduced receptor count
In cats, DM typically results from beta-cell degeneration in the pancreas, linked to conditions affecting insulin receptor sensitivity: - Pancreatitis
- Chronic inflammatory diseases
- Obesity
- Hormonal disorders
Consequences of Insulin Deficiency:
- Blood glucose rises (hyperglycemia)
- Cells experience glucose shortage
- Excess glucagon worsens imbalance Cells break down stored glycogen and fat (TAG) into glucose and fatty acids. Fatty acids undergo β-oxidation in mitochondria, forming Acetyl-CoA:
- Some enters the Krebs Cycle
- Some converts to ketone bodies (acetoacetate, beta-hydroxybutyrate, acetone)
Excess ketone bodies cause blood acidity (acidosis), disrupting acid-base balance—a condition termed ketoacidosis.
When blood glucose exceeds renal threshold:
- Excess glucose excreted in urine (glucosuria)
- Increased urine volume/density (polyuria)
- Elevated plasma osmolality and thirst (polydipsia)
Diagnosing Diabetic Ketoacidosis in Cats
Diagnostic Criteria for DKA
DKA is confirmed when all three conditions coexist:
- Hyperglycemia: Elevated blood glucose
- Ketones: Ketone bodies in blood/urine
- Acidosis: Blood pH < 7.35 (normal pH: 7.4)Note: ~10% cases show normal glucose (“Euglycemic DKA”).
pH Measurement Protocol
- Sample Type: Venous blood is sufficient (minimal arterial-venous pH difference)
- Sampling Caution: Repeated draws risk anemia; use ear vein collection for minimal invasiveness
Glucometer Use for DKA Cat Bloodwork
AlphaTRAK 2 Glucometer (Zoetis):
- Species-specific calibration for cats/dogs
- Requires only 0.3 μL blood
- Technique: Light ear margin prick with 25G needle
Read More About : AlphaTRAK 2 Glucometer
Ketone Testing in Cats
| Ketone Testing in Cats | ||
| Testing Method | Ketone Detected | Reliability |
|---|---|---|
| Urine | Acetoacetate | Less accurate |
| Blood | β-hydroxybutyrate | Highly accurate |
| Diabetic Ketoacidosis in Cats: The Rajasthan Express | ||
- Blood β-hydroxybutyrate levels indicate hospitalization needs.
- ⚠️ Degrades rapidly—test immediately after collection.
DKA Cat Bloodwork Essentials
| DKA Cat Bloodwork Essentials | |
| Test | Purpose |
|---|---|
| Urea, Creatinine | Kidney function |
| Electrolytes (Na⁺, K⁺, Cl⁻, HCO₃⁻) | Acid-base balance |
| CBC | Infection/inflammation screening |
| CRP | Acute infection marker |
| Amylase/Lipase | Pancreatitis detection |
| Urinalysis + Culture | UTI confirmation |
| Chest X-ray | Rule out lung infection |
| Diabetic Ketoacidosis in Cats: The Rajasthan Express | |
DKA vs. HHS (Hyperosmolar Hyperglycemic State)
| DKA vs. HHS (Hyperosmolar Hyperglycemic State) | ||
| Feature | DKA | HHS |
|---|---|---|
| Ketones | Markedly elevated | Minimal/absent |
| pH | < 7.35 | Normal/mildly decreased |
| Plasma Osmolarity | Normal/moderate | Very high (>320 mOsm/kg) |
| Glucose Level | 300–600 mg/dL | 600–1200 mg/dL |
| Diabetic Ketoacidosis in Cats: The Rajasthan Express | ||
Summary:
DKA diagnosis requires:
- Hyperglycemia
- Blood/urine ketones
- Acidosis (↓ pH)
Additionally, screen for: - Infections
- Kidney function
- Electrolyte imbalances
These factors dictate treatment plans and prognosis.
Learn critical DKA symptoms in cats, bloodwork diagnostics, vet treatments & survival rates. Expert-backed guide to saving your cat’s life during this metabolic emergency.
THE RAJASTHAN EXPRESS
Frequently Asked Questions About Diabetic Ketoacidosis (DKA) in Cats
Can diabetic ketoacidosis in cats resolve without veterinary treatment?
No. DKA is invariably fatal without intensive treatment due to:
- Severe dehydration and electrolyte imbalances 18
- Progressive metabolic acidosis causing organ failure 26
- Risk of cerebral edema or cardiac arrhythmias 13
- Survival rates drop to <10% without intervention; hospitalization with IV fluids, insulin, and electrolyte correction is essential 38.
Why does my diabetic cat’s breath smell sweet during a DKA crisis?
- Exhaled acetone: A volatile ketone body produced during fat metabolism 36
- Ketonemia: Blood ketone concentrations >2.5 mmol/L overwhelm buffering systems, releasing acetone via respiration 613.
- This sign indicates severe ketoacidosis requiring immediate care 1.
Do Siamese or Abyssinian cats have higher DKA mortality rates?
No breed-specific mortality data exists for DKA. Prognosis depends on:
- APPLEfast scores >24.5 4
- Blood glucose >358 mg/dL at admission 4
- Concurrent organ failure (e.g., kidney disease) 613.
- Breed is not a documented risk factor in current literature.
Financial cost of DKA treatment: When is euthanasia the only option?
Treatment typically costs $3,000–5,000 due to:
- 3–7 days of ICU care 11
- Frequent lab monitoring (electrolytes, blood gases) 6
Euthanasia may be considered if:
- Underlying conditions (e.g., cancer, end-stage kidney disease) are untreatable 8
- Survival probability is <30% (e.g., APPLEfast >30, coma) 411.
Can cats have normal blood glucose during DKA?
Yes, in euglycemic DKA:
- Blood glucose 90–250 mg/dL despite ketoacidosis 510
- Caused by SGLT2 inhibitors (e.g., Bexacat®, Senvelgo®) 15
- Diagnosed via blood ketones (β-hydroxybutyrate >2.4 mmol/L) + acidosis (pH <7.35) 213.
- Requires immediate insulin—even without hyperglycemia 10.
Why do 70% of DKA cats develop pancreatitis or liver disease concurrently?
Pathophysiological links include:
- Pancreatitis: Inflamed pancreas reduces insulin secretion, worsening hyperglycemia 611
- Hepatic lipidosis: Fat mobilization overloads the liver with triglycerides 313
- Stress hormones: Cortisol/epinephrine from inflammation promote insulin resistance 26.
- Screening via fPLI (pancreatitis) and liver enzymes is critical 6.
DKA survival rates: How age and kidney values predict outcomes
Survival rate: 70% with aggressive care 8
Poor prognostic indicators:
| Factor | Impact |
|---|---|
| Age >10 years | Reduced organ reserve 4 |
| Creatinine >2.5 mg/dL | Indicates kidney dysfunction 413 |
| APPLEfast score >24.5 | 1.08x increased mortality per point 4 |
| Acidosis (pH <7.0) | doubles mortality risk 6 |
Low-carb wet food vs. prescription diets for preventing DKA relapse
- Low-carb wet food: Reduces glucose spikes; suitable for early diabetes 16
- Prescription diets (e.g., Hill’s m/d):
- Formulated with controlled fiber/protein to stabilize glucose 1
- Clinically proven to support remission in 25–40% of cats 36
- Key: Transition under vet guidance; never fast diabetic cats 10.
At-home ketone testing: Urine strips vs. blood meters
| Method | Pros | Cons |
|---|---|---|
| Urine strips | Low cost; detects acetoacetate | Misses early ketosis; 18% false negatives 6 |
| Blood ketometers (e.g., Precision Xtra) | Measures β-hydroxybutyrate (key DKA ketone); >95% accuracy 213 | Higher cost; requires ear-prick sampling |
Recommendation: Blood testing 2x/week for diabetic cats 15.
Can diabetic remission occur after DKA in cats?
Yes, but challenging:
Remission requires:
- Early insulin therapy (glargine preferred) 6
- Low-carb diet + weight management 3
- Resolution of concurrent illness (e.g., UTI) 8
Only 15–25% of DKA survivors achieve remission vs. 40% in uncomplicated diabetes 36.