Uterine Infections in Cattle: A Comprehensive Guide to Metritis, Endometritis, and Pyometra
Introduction and Causes of Uterine Infections
Uterine infection, also known as postpartum uterine inflammation (Postpartum Metritis) or Endometritis, is primarily an inflammation of the inner lining of the uterus caused by a bacterial infection after calving or abortion. Uterine infections are a serious problem that affects the dairy industry and livestock farmers economically, directly impacting fertility and increasing the calving interval.
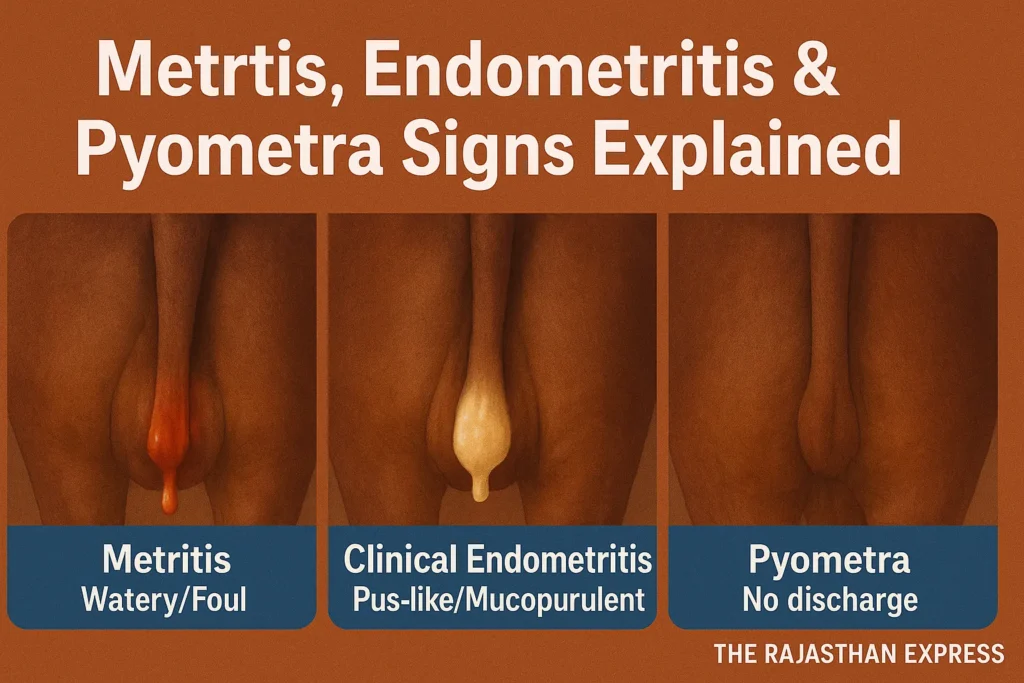
Metritis: This is a deep inflammation of the uterus occurring immediately after calving (puerperal period). The animal shows general symptoms like fever and lethargy. The uterus becomes enlarged and produces a watery or pus-like (purulent) discharge.
Endometritis: This is an inflammation of the inner lining of the uterus (Endometrium). After calving, there is a pus-like discharge, but the animal appears normal. In sub-clinical endometritis, no external discharge is visible, only inflammatory cells are found in the uterus.
Pyometra: In this condition, the infection becomes closed inside the uterus and fills with pus. This situation occurs due to the persistence of the corpus luteum and often produces symptoms similar to pregnancy.
Time of Infection: This infection usually occurs within the first 24 hours to 10 days after calving.
Main Causes of Infection: Uterine infection is mainly caused by bacteria, such as E. coli, Arcanobacterium pyogenes, and Fusobacterium species. In some cases, fungi like Candida and Aspergillus can also be responsible.
Main Symptoms: Symptoms such as fever (over 38.0 °C), chills, pain in the lower abdomen, and foul-smelling vaginal discharge can be observed.
Complications: If not treated in time, this infection can lead to serious complications like temporary infertility, Pelvic Inflammatory Disease (PID), abscess in the pelvic region, and life-threatening septicemia.
Uterine Infections in Cattle (Metritis Complex)
| Disease Name | Postpartum Uterine Disease (Metritis Complex) |
|---|---|
| Other Names / Synonyms | Metritis Complex, Endometritis, Whites, Puerperal Metritis, Pyometra |
| Primary Types & Definitions |
|
| Causes & Pathogens | Bacterial infection following contamination of the uterus after calving. A wide range of bacteria are involved, including Escherichia coli, Arcanobacterium pyogenes, Staphylococcus spp., Streptococcus spp., and Fusobacterium spp. . |
| Key Risk Factors |
|
| Symptoms & Clinical Signs |
|
| Diagnostic Methods |
|
| Treatment Options |
|
| Prevention Methods |
|
| Complications & Prognosis |
|
| Frequency / Prevalence | Uterine disease affects about half of all dairy cows. Metritis can affect up to 40% of cows, while clinical endometritis affects about 16.9-20%. Pyometra has a relatively low prevalence of less than 2% . |
| Economic Impact | Major economic costs due to lower milk yield, decreased pregnancy rate, higher chances of premature culling, and increased replacement costs. |
| Sources: PMC (NIH) Literature Review, Peer-Reviewed Journal Articles on Diagnostics.& The Rajasthan Express | |
Main Point:
- The E. Coli bacteria causes the disease called Colibacillosis in newborn calves, kids, piglets, lambs, etc., which is also known as white-yellow scours in calves.
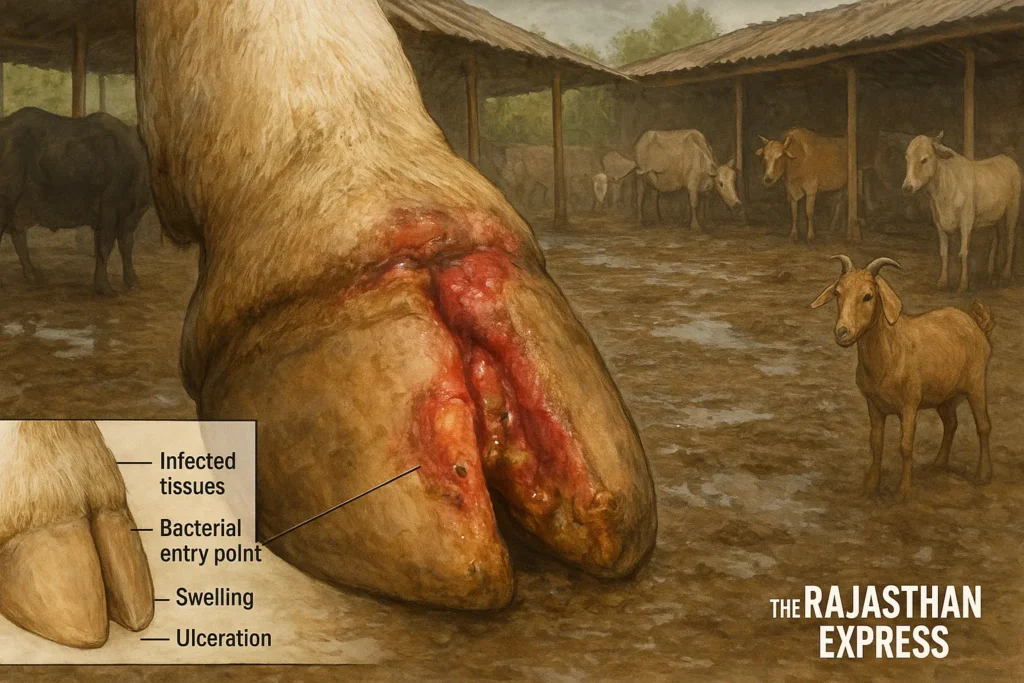
- The main causative agents of Foot Rot in cows, buffaloes, and sheep-goats are the bacteria Fusobacterium necrophorum, Dichelobacter nodosus (especially in sheep), and Bacteroides melaninogenicus (more common in cows).



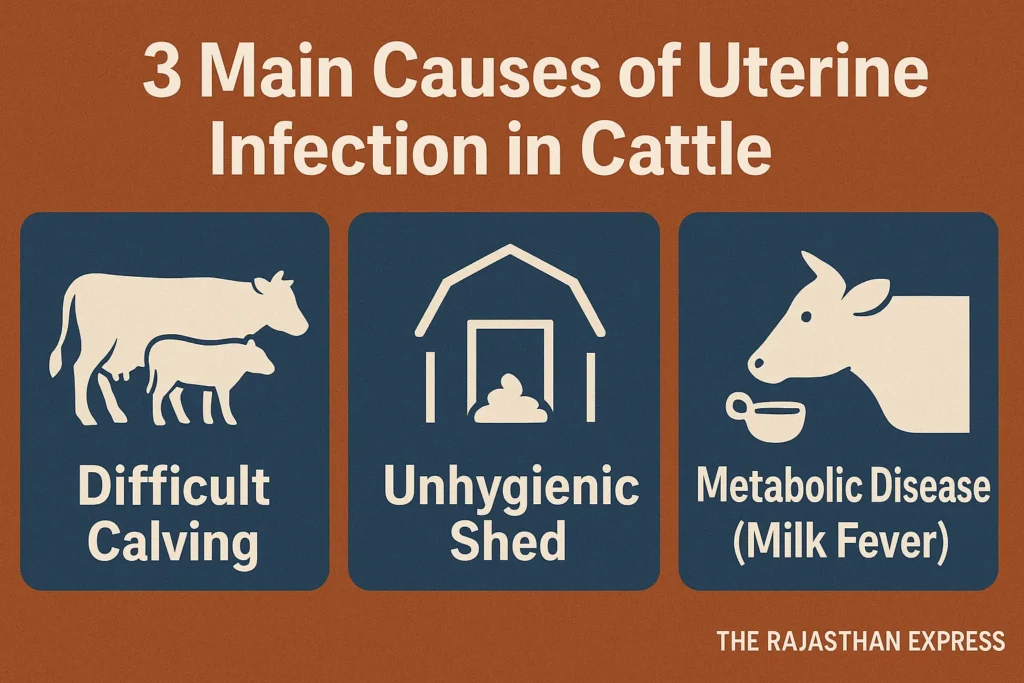
Key Predisposing Factors for Uterine Infection
The risk factors for uterine infection can be divided into three main categories. The table below clearly illustrates these factors:
| Cause of Uterine Infection in Cow & Buffalo | ||
| Type of Factor | Specific Examples | Brief Explanation |
|---|---|---|
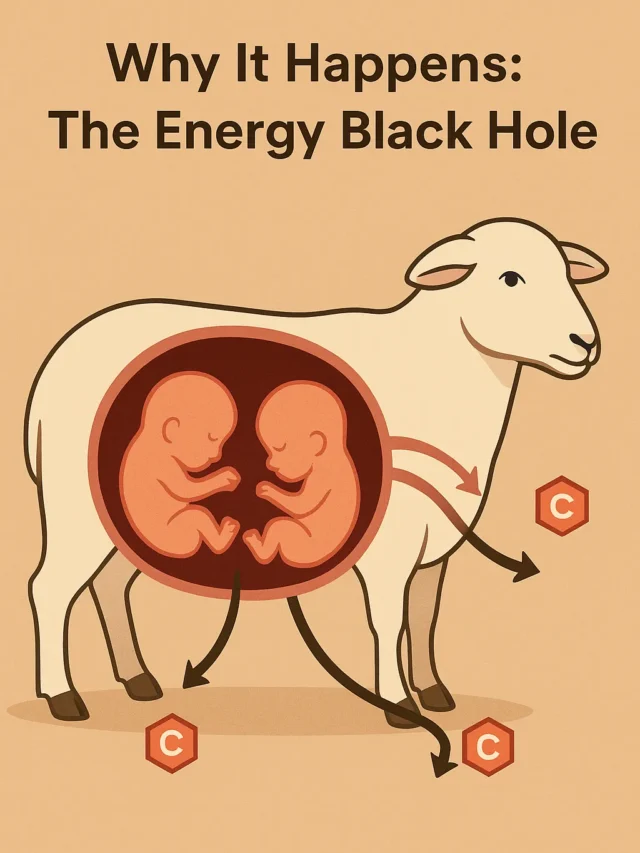
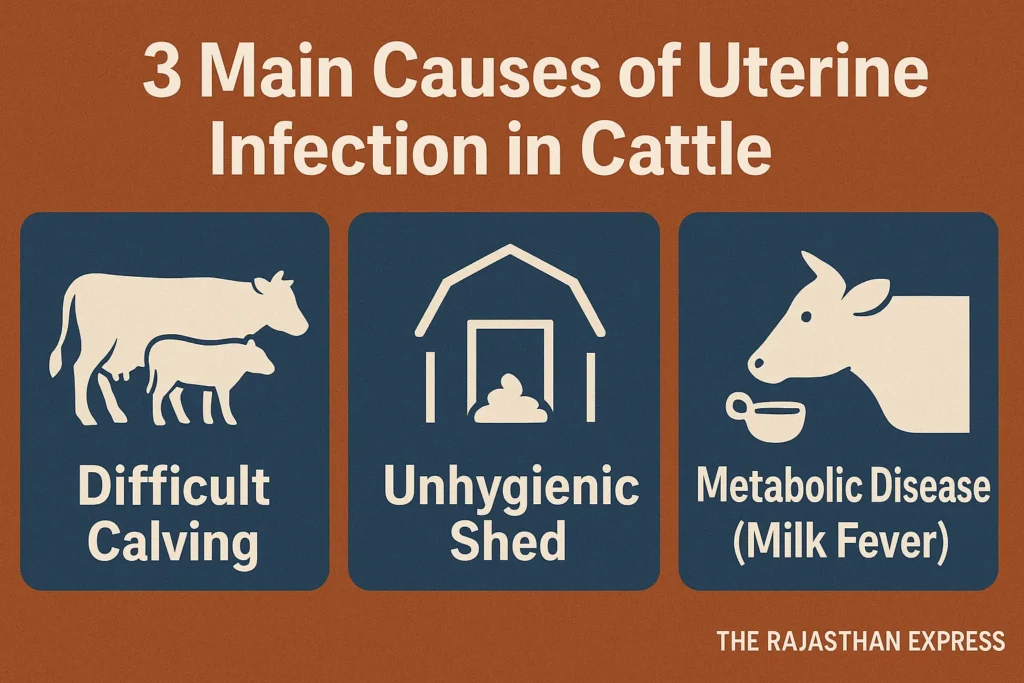
| Calving and Obstetric-Related Factors | Difficult calving (Dystocia), Retained Placenta, Prolonged calving, Premature Birth, Abortion, Foetal Maceration, Caesarean Section, Uterine Inertia (in sheep) | These conditions open the cervix or weaken the tissues, increasing the risk of bacterial entry and infection. |
| Management and Environmental Factors | Unhygienic conditions at the time of calving, injury during artificial insemination, genital tract laceration, lack of exercise, lactational stress | Poor hygiene and physical stress weaken the body’s immunity and pave the way for bacterial spread. |
| Metabolic Diseases and Dietary Management | Ketosis, Hypocalcemia (Milk Fever), Overfeeding during the Dry Period | These conditions disrupt the body’s metabolic balance, affecting uterine contraction and its ability to fight infection. |
| The Rajasthan Express : Understanding the Root Causes of Uterine Infections in Dairy Animals | ||
The Principle of Clinical Signs in Uterine Infection
The symptoms of uterine infection primarily depend on two things:
- The depth and location of the infection: Is the infection affecting the entire uterine wall or only its inner lining (endometrium)?
- The body’s general response: Is the infection so severe that it has activated the body’s entire immune system (Systemic Illness), or is the infection localized?
The table and description below clarify these differences.
| Early Detection of Uterine Infection in Cow & Buffalo: Metritis, Endometritis & Pyometra Signs | ||||
| Type of Infection | Main Symptoms | Systemic Symptoms (Affecting the Whole Body) | Uterine Condition | Vaginal Discharge |
|---|---|---|---|---|
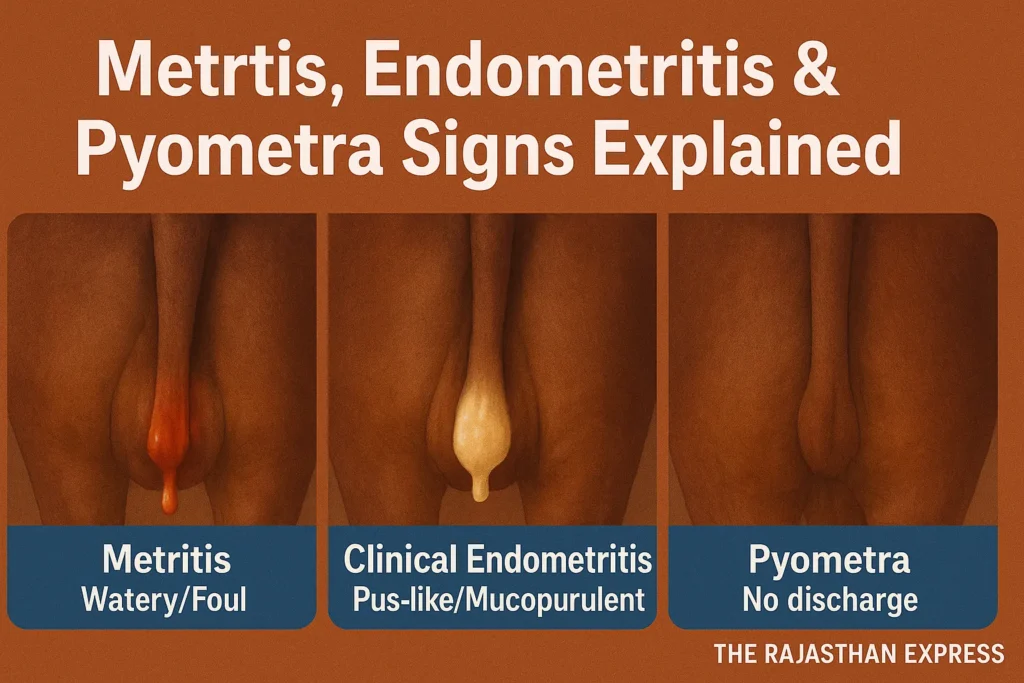
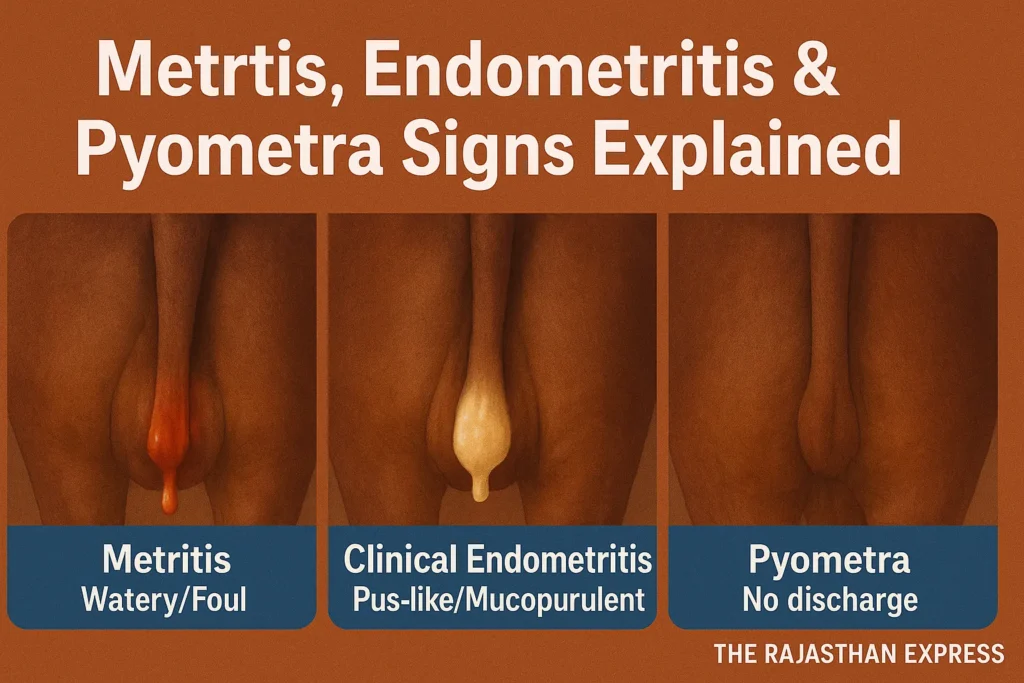
| Metritis | Acute, severe infection | Yes – Fever, lethargy, reduced appetite | Enlarged, swollen | Watery or purulent, often foul-smelling |
| Clinical Endometritis | Mild to moderate infection | No – The animal otherwise appears normal | Normal or slightly enlarged | White-yellow pus or mucopurulent discharge |
| Sub-clinical Endometritis | Hidden infection | Absolutely not – No external symptoms | Normal | No abnormal discharge seen |
| Pyometra | Collection of pus in a closed uterus | No (initially), but lethargy may occur later | Enlarged, filled with pus | Usually no discharge (because the cervix remains closed) |
| The Rajasthan Express : Understanding Clinical Signs of Uterine Infection | ||||
In-Depth Information on the Symptoms of Each Condition
1. Metritis – Deep Inflammation of the Uterus
This is the most severe infection occurring right after calving (in the postpartum period).
- Systemic Illness: The infection spreads throughout the body. The animal shows symptoms like high fever (103-105°F), severe lethargy, and reduced appetite (Anorexia).
- Dehydration: Due to fever and reduced eating/drinking, the animal may become dehydrated.
- Drastic drop in milk production.
- Uterine Condition: On rectal palpation, the uterus feels very large, flabby, and swollen.
- Vaginal Discharge: There is a watery, red-brown, or pus-like discharge with a strong, rotten fish-like odor.
2. Clinical Endometritis – Inflammation with Apparent Symptoms
This condition is less severe than metritis and is usually seen 3-4 weeks after calving.
- No Systemic Symptoms: The animal does not have a fever and eats and drinks normally. This is its biggest difference from metritis.
- Vaginal Discharge: The most prominent symptom is purulent discharge.
- Purulent: Cloudy, white-yellow pus.
- Mucopurulent: Pus mixed with mucus, making it thick and sticky.
- This discharge usually has no odor or very little odor.
- Irregular Estrous Cycle: The animal’s heat cycle is disrupted, or it fails to conceive despite repeated heat cycles (Repeat Breeding).
3. Sub-clinical Endometritis – The “Invisible” Infection
This is the most difficult condition because no external symptoms are visible.
- No External Symptoms: The animal appears completely healthy, has no fever, and shows no abnormal vaginal discharge.
- Hidden Problem: Inflammatory cells are present inside the uterine lumen, which impair fertility.
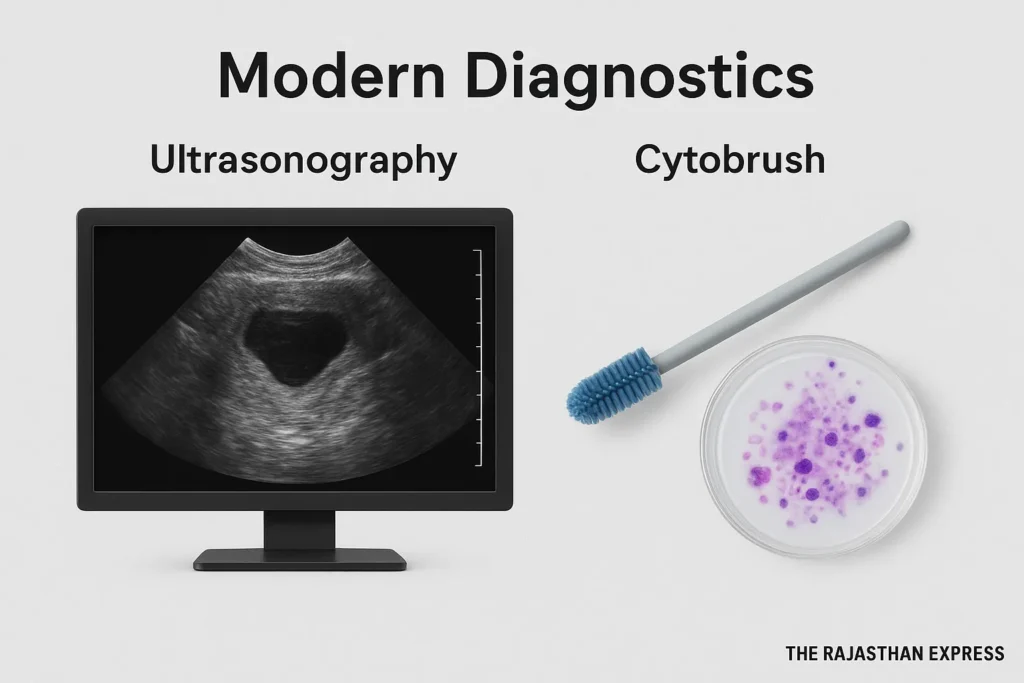
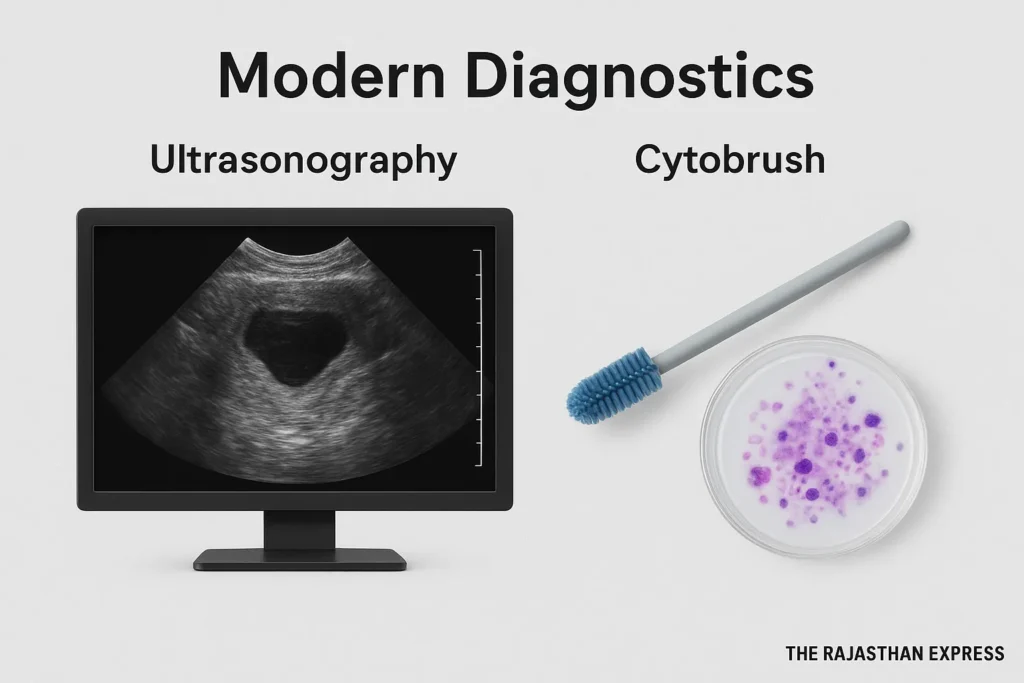
- Diagnosis: Special tests are needed to detect it, such as:
- Ultrasonography: Viewing fluid or abnormalities in the uterus.
- Cytobrush Cytology: Taking a sample of uterine cells and examining them under a microscope.
- White Side Test: Detecting the presence of white blood cells in the discharge.
4. Pyometra – Pus in a Closed Uterus
In this condition, the cervix closes, trapping the pus formed inside the uterus.
- No Discharge: Since the cervix remains closed, there is no vaginal discharge. This is its most distinctive identification.
- Uterine Condition: On rectal palpation, the uterus feels as large as a watermelon or a ball, tense, and filled with fluid.
- Estrous Cycle Stops: Due to the infection, a corpus luteum persists in the uterus, preventing the animal from coming into heat again (Anestrus).
- Normal but Infertile: The animal may appear healthy but cannot conceive. If it persists for a long time, the animal may become lethargic and its milk production may decrease.
Modern Diagnostic Methods for Uterine Infection
Along with diagnosis based on traditional symptoms, modern medical science has developed highly accurate methods for detecting uterine infections, especially sub-clinical endometritis.
1. Traditional Methods
- Rectal Palpation: Diagnosis of metritis, endometritis, or pyometra is usually based on rectal palpation and observation of discharge patterns. However, diagnosing endometritis, especially subclinical endometritis, through rectal palpation is challenging because the size of the uterus and its consistency vary significantly between different animals, making the assessment entirely subjective. Consequently, rectal palpation often proves to be an inadequate method for detecting subclinical endometritis.
- Endometritis Clinical Score: The purpose of the Endometritis Clinical Score is to assess the severity of the infection based on the nature of the vaginal discharge and other symptoms. It is a systematic method doctors use to grade the condition. This method functions similarly to how the Body Condition Score works in cows and buffaloes.
- Assessment of Symptoms: This primarily focuses on the vaginal discharge. The discharge’s color (yellow, green), consistency (thickness), and odor (foul-smelling) indicate infection.
- Physical Examination: During a pelvic examination, the doctor assesses the size, tenderness, and swelling of the uterus. A tender or swollen uterus can be a symptom of endometritis.
- Scoring System: Different symptoms are assigned points. For example, normal discharge may be scored 0 points, mildly purulent (pus-containing) discharge may be scored 1 point, and heavily purulent discharge may be scored 2 points. Based on these points, the severity of the infection (mild, moderate, severe) is determined, which clarifies the path for treatment.
2. Laboratory-Based Diagnostics
- Endometrial Cytology: This involves taking a sample of cells from the inner lining of the uterus using a cytobrush or lavage technique and analyzing them under a microscope. If the number of Polymorphonuclear Neutrophil (PMN) cells is found to be above a certain percentage (e.g., 5%), it is a clear sign of inflammation.
- Bacterial Culture and Drug Sensitivity: A sample of vaginal or uterine discharge is taken and cultured. This identifies the specific bacteria causing the infection and allows for a drug sensitivity test to determine which antibiotic will be most effective.
- Histopathological Examination: A small sample of uterine tissue is taken via endometrial biopsy and examined under a microscope. This method is considered extremely accurate in confirming the state of inflammation in the tissues.
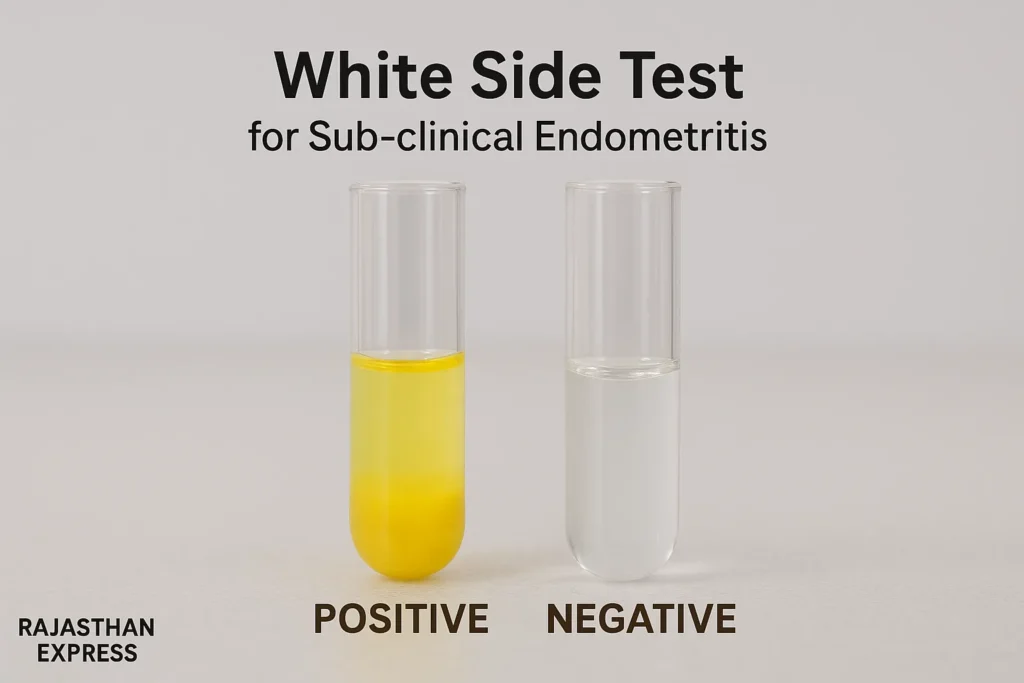
The White Side Test for Endometritis in Cattle
The White Side Test is a simple and quick diagnostic test primarily used in the field of veterinary medicine. This test is specifically conducted in cows and buffaloes to detect endometritis or genital infection, which is a major cause of repeat breeding failure.
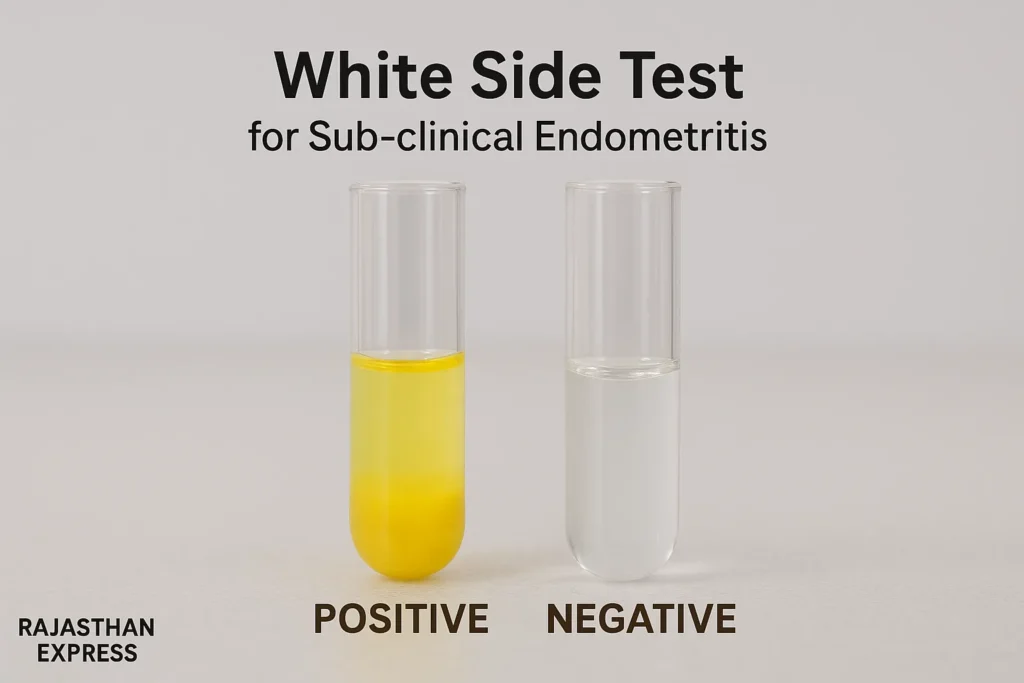
- Actual Purpose (in Veterinary Medicine): This test detects the increased amount of inflammatory cells, specifically white blood cells (Leukocytes) and protein, present in the cervical mucus, which is an indicator of infection.
- Procedure:
- Sample: A mucus sample is collected from the cervix during the animal’s estrus.
- Chemical: The mucus sample is mixed with an equal amount of 5% Sodium Hydroxide solution in a test tube.
- Boiling and Cooling: The mixture is heated to the boiling point and then cooled.
- Result: The color change and consistency resulting from the reaction are observed.
- Interpretation of Results:
- Negative (Normal): If there is no infection in the mucus, the color of the mixture remains unchanged.
- Positive (Infection): If there is an excess of white blood cells, the color of the mixture changes from light yellow to deep yellow, indicating the severity of the infection. This color change is due to the presence of protein released from the breakdown of white blood cells.
- Importance:
- It is a cost-effective and rapid test performed at the field level.
- It is used specifically for the diagnosis of subclinical endometritis, where the animal shows no external symptoms of infection.
Main Point:
- When an injury occurs in any part of the body or a germ (like bacteria) enters, neutrophils are the first white blood cells to rapidly reach the site of infection or injury by leaving the blood vessels.
- The main function of neutrophils is to engulf and destroy invading germs. They release enzymes and other toxic chemicals to do this. This very action causes local inflammation.
- Increased Count: When there is acute inflammation or a bacterial infection anywhere in the body, the body increases the production of neutrophils and sends them rapidly into the bloodstream. An increased number of neutrophils in a blood test is called Neutrophilia and is a clear sign of infection.
- Read More About : WHITE SIDE TEST FOR CATTLE & BUFFALO
3. Imaging-Based Diagnostics
- Ultrasonography: This is the most important and crucial method of modern diagnosis. It accurately reveals the internal structure of the uterus, the presence of fluid, pus, abscesses, and the thickness of the uterine wall. In conditions like pyometra, the uterus appears filled with fluid and distended.
- Vaginoscopic Examination: Using a telescope-like device, the vaginal passage and cervix are directly examined, allowing assessment of the nature and quantity of discharge.
4. Emerging and Advanced Techniques
- Molecular Techniques: Sensitive techniques like Polymerase Chain Reaction can be used to detect the DNA of the bacteria responsible for the infection, even if their numbers are very low.
- Biomarker Discovery: Current research is focused on identifying specific biomarkers, such as proteins or miRNAs, present in blood or uterine discharge that can provide early information about the infection.
Treatment for Endometritis, Metritis, and Pyometra
The goal of modern treatment is to cure the infection while avoiding antibiotic residues in milk and enhancing the animal’s own immune capacity.
1. Choice of Medications
- Antibiotics: Antibiotics such as ceftiofur, cephapirin, amoxicillin, etc., are used. A drug sensitivity test is essential to determine which antibiotic is effective.
- Hormone Therapy: Prostaglandin F2α is used in pyometra and endometritis. It helps by increasing uterine contractions to expel the infected material.
- Anti-inflammatory Drugs: Drugs like flunixin meglumine or meloxicam help the animal recover faster by reducing inflammation and pain.
2. Antibiotic Alternatives and Immunomodulation
- Challenge of Antibiotic Resistance: Antibiotic resistance is a major problem worldwide, hence research on alternative treatments is ongoing.
- Immunomodulators: These are substances that boost the animal’s own immunity. These include:
- Extracts of herbs like Giloy and Neem oil.
- Colostrum whey and hyperimmune serum.
- Molecules like Granulocyte-Macrophage Colony-Stimulating Factor, which stimulate the production of white blood cells.
| 💊 Immunity Boosting Components (Immunomodulators) | |||
| Category | Immunomodulator | Main Mechanism & Effect | Examples & Research Findings |
|---|---|---|---|
| Natural / Herbal | Yu Ping Feng Polysaccharides (YPF-P) A natural immunomodulator derived from a Traditional Chinese Medicine (TCM) formulation. | Increases serum antibody levels; regulates CD4+/CD8+ ratio; enhances both Humoral and Cell-Mediated Immunity. | Improves survival in pigs, growth in poultry, and milk yield in cows; acts as a vaccine adjuvant. Source: Frontiers in Veterinary Science, 2024 |
| Natural / Herbal | Ashwagandha Root Extract (Withania somnifera) – also called Indian Ginseng or Winter Cherry. Contains Withanolides, Alkaloids, and Saponins. | Reduces cortisol (stress hormone); increases immune cells (TEC, TLC); has strong antioxidant and adaptogenic properties. | Improves stress tolerance in horses; enhances immunity and resilience. Source: Journal of Ethnopharmacology, 2020 |
| Natural / Herbal | Other Plant Polysaccharides (e.g., Astragalus) | Regulates cytokine expression (IL-1β, IL-2, IFNγ); promotes macrophage and lymphocyte proliferation. | Improves antibody response in poultry vaccines (Newcastle Disease, Avian Influenza). Source: Frontiers in Immunology, 2021 |
| Natural / Herbal | Chinese Herbal Mixture (CHMM) Polyherbal TCM formulation typically including Astragalus, Licorice (मुलेठी), Angelica, and Ginseng extracts. | Upregulates immune genes (NF-κB, TNF-α, IFN-β); enhances antioxidant enzyme activity. | Increases immune response and antiviral resistance in Rainbow Trout. Source: Aquaculture Research, 2022 |
| Probiotics & Microbiota-Targeted | Specific Probiotic Formulation Examples: Lactobacillus, Bifidobacterium, Enterococcus | Improves gut health and strengthens immune regulation via microbiota modulation. | Enhances antibody response in animals; reduces gut infections. Source: Frontiers in Microbiology, 2019 |
| Probiotics & Microbiota-Targeted | Microbiota-Targeted Feed Additives (Prebiotics + Probiotics + Herbal combinations) | Balances beneficial gut bacteria; promotes systemic immunity through microbiota–immune axis. | Improves vaccine efficacy (e.g., Rabies in mice). Source: Frontiers in Microbiology, 2019 |
| Pharmaceuticals | Glucocorticoids | Suppresses cell-mediated immunity; inhibits pro-inflammatory cytokines (IL-1, IL-2, IL-6, TNFγ). | Used for autoimmune disorders and organ transplant rejection. Source: Veterinary Pharmacology (Giguère et al., 2018) |
| Pharmaceuticals | Cytostatic Drugs (e.g., Cyclophosphamide) | Inhibits cell division; exhibits strong immunosuppressive properties. | Used in Systemic Lupus Erythematosus and Autoimmune Hemolytic Anemia. Source: Merck Veterinary Manual, 2023 |
| Pharmaceuticals | Levamisole | Activates both Th1 and Th2 immune pathways; boosts macrophage and T-lymphocyte activity. | Improves vaccine response and disease resistance in cows, sheep, and poultry. Source: Veterinary Immunology and Immunopathology, 2014 |
| Nutritional / Vitamins | Vitamin C (Ascorbic Acid) | Powerful antioxidant; neutralizes ROS; enhances neutrophil function and antibody production. | Reduces heat stress in poultry and calves; strengthens immunity. Source: Journal of Dairy Science, 2011 |
| Nutritional / Vitamins | Vitamin E (α-Tocopherol) | Prevents lipid peroxidation; protects cell membranes; enhances cytokine and antibody production. | Increases disease resistance in poultry; reduces mastitis in dairy cows. Source: Poultry Science, 2018; Journal of Animal Science, 2013 |
| The Rajasthan Express : Natural and Scientific Immunomodulators in Veterinary Practice | |||
Read More About : Boosting Milk Production After Lumpy Skin Disease
3. Supportive Treatment
- Administering an Oxytocin injection immediately after calving causes uterine contractions, which reduces the problem of retained placenta and the likelihood of infection.
- Providing fluid therapy, calcium, and energy-rich supplements is beneficial for weak animals.
Prevention and Control Measures
Preventing uterine infections is better and more cost-effective than treatment. A uterine infection prevention strategy should include the following:
- Balanced Dietary Management: Provide the animal with a balanced diet before and after calving. Prevent deficiencies in calcium and energy, as this increases the risk of retained placenta.
- Clean Housing and Calving Management: Provide a clean, dry, and sufficiently large pen for calving. Follow strict hygiene during calving.
- Regular Health Monitoring: Conduct regular check-ups of animals after calving. Use modern techniques like ultrasound or cytobrush to detect sub-clinical endometritis.
- Early Intervention: Research is ongoing on the use of immunomodulators immediately after calving, which can prevent the infection at the outset.
Summary of the Entire Article
Uterine infections are a major challenge for the economic stability of dairy farms. To overcome them, it is essential to focus on prevention, adopt modern and accurate diagnostic methods, and carefully use antibiotics along with alternative treatments like immunomodulators. An integrated approach is the key to success in increasing farm productivity and reducing the calving interval.
Learn 4 easy methods for the early detection of Uterine Infection (Metritis, Endometritis, Pyometra) in cow and buffalo. Use Metricheck, White Side Test, and postpartum symptoms to prevent infertility.
THE RAJASTHAN EXPRESS